Thalassemia: An Overview
What is Thalassemia?
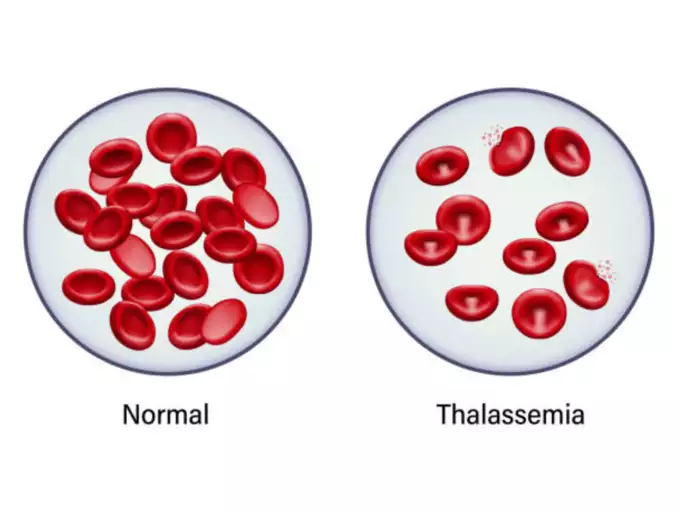
Thalassemia is a genetic blood disorder characterized by the body’s inability to produce normal amounts of hemoglobin, the protein in red blood cells responsible for transporting oxygen. This deficiency can lead to anemia, which often results in feelings of exhaustion.
Managing Mild and Severe Thalassemia
Individuals with a mild form of thalassemia may not require any medical intervention. However, those with more severe conditions are likely to need regular blood transfusions. Adopting a nutritious diet and maintaining an active lifestyle can help alleviate fatigue associated with the disorder.
Recognizing the Symptoms
The symptoms of thalassemia vary based on its type and severity and may include:
- Fatigue and Weakness
- Skin Discoloration (pale or yellowish tone)
- Deformities in Facial Bones
- Stunted Growth
- Abdominal Distension
- Discolored Urine
While some infants may exhibit symptoms at birth, others may develop them within the first two years. It’s also possible for individuals with a single mutated hemoglobin gene to show no symptoms at all.
When to Consult a Doctor
Should your child display any symptoms indicative of thalassemia, it is crucial to schedule a consultation with a pediatrician for a thorough assessment.
Understanding Thalassemia Causes
Genetic Roots of Thalassemia
Thalassemia arises from genetic mutations in the DNA of cells tasked with producing hemoglobin — the vital molecule in red blood cells that distributes oxygen throughout the body. These mutations are hereditary, passed down from parents to offspring.
Hemoglobin Structure and Thalassemia
Hemoglobin is composed of alpha and beta chains, and mutations can impair either, leading to two main types of thalassemia: alpha-thalassemia and beta-thalassemia. The production levels of these chains are crucial, as their reduction is directly linked to the disease.
Alpha-Thalassemia and Its Impact
The severity of alpha-thalassemia depends on the number of mutated genes inherited:
- One mutated gene: Typically asymptomatic, but you’re a carrier.
- Two mutated genes: Mild symptoms, known as alpha-thalassemia trait.
- Three mutated genes: Moderate to severe symptoms.
- Four mutated genes: Often leads to stillbirth or requires intensive treatment post-birth.
Beta-Thalassemia and Its Variations
Beta-thalassemia’s severity is influenced by the specific part of the hemoglobin molecule affected:
- One mutated gene: Mild symptoms, referred to as thalassemia minor or beta-thalassemia.
- Two mutated genes: Moderate to severe symptoms, known as thalassemia major or Cooley anemia.
Newborns with two defective beta hemoglobin genes typically appear healthy but develop symptoms within the first two years. Thalassemia intermedia is a less severe form resulting from two mutated genes.
Thalassemia: Risk Factors and Prevention
Identifying Risk Factors
The likelihood of developing thalassemia is influenced by:
- Family History: Inheritance of mutated hemoglobin genes from parents.
- Ethnic Background: Higher prevalence in African Americans, and individuals of Mediterranean and Southeast Asian descent.
Potential Complications
Moderate to severe thalassemia can lead to:
- Iron Overload: Excessive iron from the disease or transfusions, damaging vital organs and endocrine system.
- Increased Infection Risk: Particularly post-splenectomy.
Severe Thalassemia Complications
- Bone Deformities: Expansion of bone marrow leading to abnormal bone structures.
- Enlarged Spleen: Overworking due to excessive red blood cell destruction.
- Growth Delays: Anemia-induced growth and puberty delays.
- Heart Issues: Risks of congestive heart failure and arrhythmias.
Prevention Strategies
While thalassemia is generally unpreventable, those affected or carrying the gene should consider:
- Genetic Counseling: For family planning and understanding risks.
- Assisted Reproductive Technology: Screening embryos for genetic mutations to ensure the birth of healthy children.
This reproductive technology involves the combination of in vitro fertilization with genetic screening, where only embryos free of genetic defects are implanted into the uterus. This process offers a proactive approach for prospective parents with thalassemia or carrier status to have unaffected offspring.
| Category | Subcategory | Details |
|---|---|---|
| Overview | Definition | A genetic blood disorder causing less hemoglobin and resulting in anemia. |
| Management | Mild cases may not need treatment; severe cases require transfusions and lifestyle adjustments. | |
| Symptoms | Variability | Depends on thalassemia type and severity; can include fatigue, bone deformities, and more. |
| Age of Onset | Some at birth, others within the first two years, or may be asymptomatic carriers. | |
| Causes | Genetic Mutations | DNA mutations in cells making hemoglobin; passed from parents to children. |
| Alpha and Beta Chains | Mutations affect the production of these chains, leading to alpha or beta thalassemia. | |
| Risk Factors | Family History | Inherited through mutated hemoglobin genes. |
| Ancestry | More common in African Americans, Mediterranean, and Southeast Asian descent. | |
| Complications | Iron Overload | From the disease or frequent blood transfusions. |
| Infection | Increased risk, especially if the spleen is removed. | |
| Prevention | Genetic Counseling | Advised for those with thalassemia or carriers. |
| Reproductive Technology | Embryo screening combined with IVF for healthy babies. | |
| Diagnosis | Blood Tests | Reveal red blood cell count and abnormalities, DNA analysis for mutated genes. |
| Prenatal Testing | Chorionic villus sampling and amniocentesis to detect thalassemia in fetuses. | |
| Treatment | Blood Transfusions | For severe cases; can lead to iron buildup. |
| Chelation Therapy | To remove excess iron from the blood. | |
| Stem Cell Transplant | For severe cases, can eliminate the need for transfusions. | |
| Self-Care | Diet and Supplements | Avoid excess iron, ensure a healthy diet, and consider supplements like folic acid. |
| Infection Prevention | Good hygiene, vaccinations, and avoiding sick people. | |
| Support | Professional Advice | Reach out to healthcare providers for guidance. |
| Support Groups | For emotional support and information. | |
| Appointment Prep | Documentation | Record symptoms, family history, and medications. |
| Questions for Doctor | Inquire about causes, tests, treatments, dietary advice, etc. | |
| Doctor’s Questions | Be prepared to discuss symptom patterns and severity. |