Anthrax: An Overview
Anthrax is an infrequent but severe bacterial illness caused by Bacillus anthracis. It predominantly affects livestock and wildlife, with human infections arising from contact with afflicted animals. While not transmissible between humans, anthrax can spread via skin lesions or contaminated objects.
Infection and Symptoms
Anthrax infection can occur through skin wounds, ingestion of tainted meat, or inhalation of spores. Symptoms vary based on the infection route and may include skin sores, vomiting, and shock. Antibiotics are effective against most forms of anthrax, but inhaled anthrax poses greater treatment challenges and can be lethal.
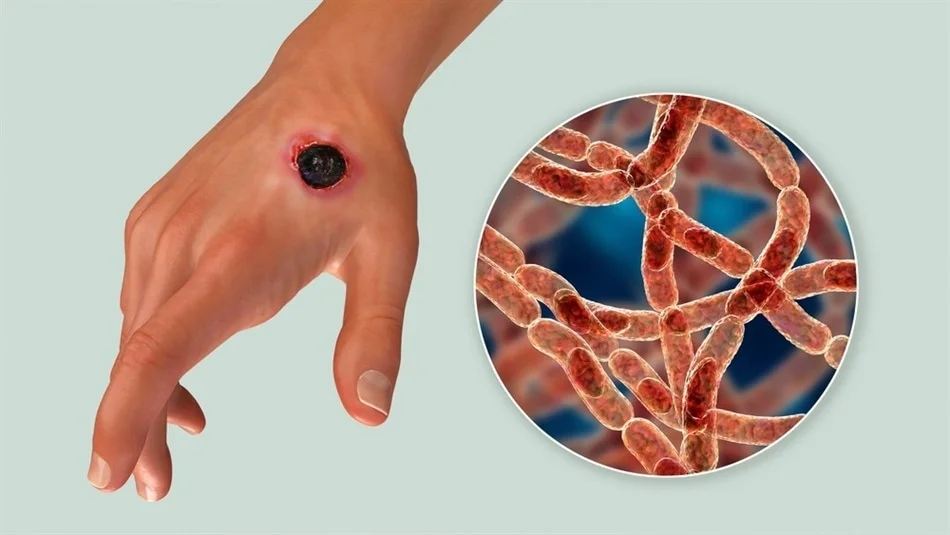
Cutaneous Anthrax
The most prevalent and least severe form, cutaneous anthrax, involves skin entry, typically through a cut. Symptoms, which are treatable and rarely fatal, may manifest as:
A raised, itchy bump that evolves into a painless sore with a black center
Swelling around the sore and lymph glands
Occasional fever and headache, resembling flu symptoms
Public Health Concerns
Despite its rarity in developed nations, anthrax remains a public health concern due to its potential use in bioterrorism, particularly in the United States.
Gastrointestinal Anthrax
Gastrointestinal anthrax arises from consuming undercooked meat from animals infected with Bacillus anthracis. It targets the digestive system from the throat to the colon. Symptoms include:
Nausea
Vomiting
Abdominal pain
Headache
Loss of appetite
Fever
Severe, bloody diarrhea in advanced stages
Sore throat and difficulty swallowing
Swollen neck
Inhalation Anthrax
Inhalation anthrax is contracted by inhaling spores and is the deadliest form, often fatal despite treatment. Early symptoms resemble the flu and escalate to severe respiratory distress:
Initial flu-like symptoms: sore throat, mild fever, fatigue, muscle aches
Mild chest discomfort
Shortness of breath
Nausea
Coughing up blood
Painful swallowing
High fever
Trouble breathing
Shock: Collapse of the circulatory system
Meningitis
Injection Anthrax
Injection anthrax, a newer form found only in Europe, is linked to injecting illegal drugs. Unlike cutaneous anthrax, it does not lead to a blackened wound but presents with:
Redness at the injection site
Significant swelling
Shock
Multiple organ failure
Meningitis
When to Consult a Doctor
Anthrax symptoms can mimic the flu, making it unlikely for common flu-like symptoms to be due to anthrax. However, if there’s a possibility of exposure, especially in high-risk environments, immediate medical evaluation is essential. Prompt attention is vital after contact with animals or animal products in regions where anthrax is prevalent.
Understanding Anthrax Causes
Anthrax spores, produced by Bacillus anthracis, are naturally present in soil globally. These spores can lie dormant for years and infect hosts like sheep, cattle, horses, and goats. While anthrax is rare in the U.S., it’s more common in the developing world, including parts of Africa, Asia, and Europe.
Human anthrax infections typically result from contact with infected animals or their products. Notably, the U.S. has seen cases related to the handling of infected animal skins for drum making. Additionally, anthrax has been used in bioterrorism, as seen in the 2001 U.S. mail attacks, and has been linked to heroin use in Europe, underscoring the disease’s diverse transmission routes.
Risk Factors for Anthrax
The risk of contracting anthrax is associated with direct contact with its spores. High-risk groups include:
Military personnel in high-risk areas
Laboratory workers handling anthrax
Individuals who process animal skins, furs, or wool in affected regions
Veterinary workers dealing with livestock
Those who handle or dress game animals
Illegal drug users, particularly of injected drugs like heroin
Complications of Anthrax
Anthrax can lead to severe complications such as:
Sepsis: The body’s abnormal response to infection, causing organ system damage
Hemorrhagic meningitis: Inflammation of brain and spinal cord membranes, potentially resulting in massive bleeding and death
Prevention Strategies
The Centers for Disease Control and Prevention (CDC) recommends the following to prevent anthrax infection:
60-day antibiotic treatment: Ciprofloxacin, doxycycline, and levofloxacin for adults and children
Anthrax vaccine: A three-dose series
Monoclonal antibodies: Raxibacumab and obiltoxaximab in certain cases
Anthrax Vaccine Information
The anthrax vaccine is designated for specific individuals and may cause side effects from mild soreness to allergic reactions. It is primarily for:
Military personnel
Anthrax researchers
People in other high-risk professions
Safety Measures
To minimize anthrax exposure:
In anthrax-prevalent regions, avoid contact with unvaccinated livestock and animal products
Do not consume undercooked meat
Exercise caution when handling dead animals or imported animal products
Category | Details |
|---|---|
Overview | A rare but serious bacterial disease, primarily affecting livestock and occasionally humans. |
Transmission | Direct or indirect contact with infected animals; not typically transmissible between humans. |
Symptoms | Varies by infection type; can include skin sores, vomiting, shock, and more. |
Types of Anthrax | Cutaneous, Inhalation, Gastrointestinal, Injection. |
Cutaneous Anthrax | Most common; symptoms include itchy bumps, sores with black centers, swelling, fever. |
Gastrointestinal | From eating contaminated meat; symptoms include nausea, abdominal pain, bloody diarrhea. |
Inhalation Anthrax | From inhaling spores; severe and often fatal, with symptoms like fever, chest discomfort. |
Injection Anthrax | Linked to injecting drugs; symptoms include redness, swelling at the injection site. |
Risk Factors | Military, lab workers, handling animal products, veterinary work, illegal drug use. |
Complications | Sepsis, hemorrhagic meningitis. |
Prevention | Vaccines, avoiding contact with infected animals, proper cooking of meat. |
Diagnosis | Based on exposure risk, symptoms; confirmed via skin testing, blood tests, imaging, stool tests. |
Treatment | Antibiotics, antitoxins, supportive care; early treatment is critical. |
When to See a Doctor | If exposed or symptoms develop after contact with animals in endemic areas. |
Causes | Anthrax spores in soil; dormant until entering a host like livestock. |
Public Health Concerns | Rare in developed countries; used in bioterrorism, linked to drug use in Europe. |