Diagnosing Transient Global Amnesia
Initial Assessment
To identify transient global amnesia (TGA), it’s essential to exclude other serious conditions that could cause similar memory loss, such as strokes, seizures, or head injuries.
Neurological Examination
The diagnostic process begins with a comprehensive neurological exam that includes:
- Reflex Checks: Evaluating reflex responses.
- Muscle Assessments: Testing muscle tone and strength.
- Sensory Tests: Checking sensory function.
- Movement Analysis: Observing gait, posture, coordination, and balance.
- Cognitive Evaluation: Questions are posed to assess thinking, judgment, and memory.
Advanced Brain Imaging Tests
Following the physical exam, further tests may be conducted to detect any irregularities in brain activity or blood flow:
- Computerized Tomography (CT): Utilizes X-rays to create detailed cross-sectional images of the brain, identifying structural abnormalities or previous strokes.
- Magnetic Resonance Imaging (MRI): Employs magnetic fields and radio waves to generate comprehensive images of the brain. An MRI might be unnecessary if a recent CT scan showed no issues.
- Electroencephalogram (EEG): Measures electrical activity in the brain through scalp electrodes. This test is particularly useful if multiple TGA episodes have occurred or if seizures are suspected.
Treatment for Transient Global Amnesia
Managing TGA
TGA typically resolves on its own without the need for treatment and is not associated with any lasting effects. The focus is on monitoring and supportive care during the recovery phase.
Preparing for a Medical Appointment: Transient Global Amnesia
Immediate Actions
In cases of sudden memory loss, emergency medical care is crucial. Dialing 911 or the local emergency number should be the first step.
Support for the Affected Individual
If you are with someone experiencing these symptoms:
- Accompany Them: Ensure they are not alone and accompany them to the hospital.
- Provide Information: As they may not recall recent events, your input is vital for the healthcare provider.
Steps You Can Take
- Stay Present: Remain with the person throughout the medical evaluation process.
- Document Events: Note any stressful events that occurred before the memory loss.
- Observe Symptoms: Keep track of any additional symptoms like numbness or weakness.
- Medical History: Inform the medical team about the person’s health history and medications.
Questions to Ask the Doctor
Prepare a list of questions such as:
- What could be causing these symptoms?
- Are there other potential causes?
- What tests are recommended?
- Is immediate treatment necessary?
- What symptoms should we watch for at home?
- When should we seek emergency help?
- How quickly will the symptoms improve?
- Can we expect a full recovery?
- How can we prevent future episodes?
- What are the risks of long-term complications?
Interaction with the Healthcare Provider
The doctor will likely inquire about:
- The individual’s last memory before the loss.
- Their awareness of personal identity.
- Recognition of accompanying persons.
- Presence of other symptoms like dizziness or vision problems.
Questions the Doctor May Ask You
Be prepared to answer questions regarding:
- The onset of memory loss.
- The progression of symptoms.
- Any prior similar incidents.
- Events preceding the memory loss.
- Any recent stressors or medical events.
- The individual’s medical history and current medications.
| Section | Key Points |
|---|---|
| Overview | – Sudden confusion in alert individuals<br>- Inability to form new memories<br>- Recognition of self and familiar people<br>- Episodes improve over hours |
| Symptoms | – Memory loss without other neurological deficits<br>- Normal cognition and awareness<br>- Symptoms last no more than 24 hours |
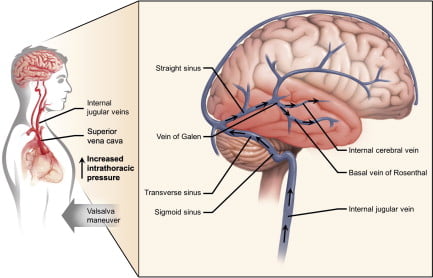
| Causes | – Unknown cause<br>- Possible link to migraines<br>- Venous congestion<br>- Triggers include physical activity, stress, medical procedures |
| Risk Factors | – Age (50+)<br>- History of migraines |
| Complications | – No direct complications<br>- Rare recurrence<br>- Emotional distress |
| Prevention | – No known prevention due to unknown cause |
| Diagnosis | – Exclusion of other conditions<br>- Neurological exam<br>- Brain imaging tests (CT, MRI, EEG) |
| Treatment | – No treatment needed<br>- Self-resolving with no lasting effects |
| Appointment Preparation | – Immediate medical attention required<br>- Accompany affected individual<br>- Provide medical history and observe symptoms<br>- Prepare questions for the doctor |
| Doctor’s Questions | – Questions about the last memory, identity, symptoms, medical history |