Diagnosing Rheumatoid Arthritis
Diagnosing rheumatoid arthritis (RA) can be challenging, especially in its early stages, as the initial signs and symptoms often resemble those of other conditions. Unlike a single definitive test, the diagnosis relies on a combination of factors.
Here’s how the diagnostic process typically unfolds:
Physical Examination: During a physical exam, your doctor will assess your joints for swelling, redness, and warmth. They may also evaluate your reflexes and muscle strength.
Blood Tests:
- Erythrocyte Sedimentation Rate (ESR) or Sed Rate: Elevated levels of ESR indicate the presence of an inflammatory process in the body.
- C-reactive Protein (CRP): Similar to ESR, an elevated CRP level suggests inflammation.
- Rheumatoid Factor (RF): This antibody is often present in individuals with RA.
- Anti-cyclic Citrullinated Peptide (anti-CCP) Antibodies: These antibodies are specific to RA and aid in diagnosis.
Imaging Tests:
- X-rays: These help track the progression of RA in your joints over time.
- MRI and Ultrasound: These imaging techniques allow your doctor to assess the severity of the disease within your body.
Remember that early detection and timely management are crucial for effectively addressing rheumatoid arthritis and minimizing its impact on your health and well-being. If you experience persistent joint symptoms, consult a healthcare professional for evaluation and appropriate care.
Treatment Options for Rheumatoid Arthritis
While there is no cure for rheumatoid arthritis (RA), early intervention with appropriate medications can significantly improve symptoms and increase the likelihood of remission. Here are the main categories of medications used to manage RA:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- NSAIDs, available both over-the-counter and by prescription, help relieve pain and reduce inflammation.
- Common examples include ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve).
- Side effects may include stomach irritation, heart issues, and kidney damage.
Steroids (Corticosteroids):
- Corticosteroid medications, such as prednisone, are effective in reducing inflammation and pain.
- They also slow down joint damage.
- Side effects may include bone thinning, weight gain, and an increased risk of diabetes.
- Doctors often prescribe corticosteroids to provide quick relief, with a gradual tapering off the medication.
Conventional Disease-Modifying Antirheumatic Drugs (DMARDs):
- These drugs slow down the progression of RA and help prevent permanent joint and tissue damage.
- Common conventional DMARDs include:
- Methotrexate (Trexall, Otrexup)
- Leflunomide (Arava)
- Hydroxychloroquine (Plaquenil)
- Sulfasalazine (Azulfidine)
- Side effects vary but may include liver damage and severe lung infections.
Biologic Agents (Biologic DMARDs):
- This newer class of DMARDs, also known as biologic response modifiers, specifically targets the immune system.
- Examples include:
- Abatacept (Orencia)
- Adalimumab (Humira)
- Anakinra (Kineret)
- Certolizumab (Cimzia)
- Etanercept (Enbrel)
- Golimumab (Simponi)
- Infliximab (Remicade)
- Rituximab (Rituxan)
- Sarilumab (Kevzara)
- Tocilizumab (Actemra)
Remember to work closely with your healthcare provider to determine the most suitable treatment plan based on your individual needs and the severity of your RA. Early diagnosis and consistent management are essential for better outcomes.
Biologic DMARDs are typically more effective when combined with a conventional DMARD, such as methotrexate. However, it’s important to note that this type of drug also increases the risk of infections.
Additionally, there are targeted synthetic DMARDs that may be considered if conventional DMARDs and biologics have not been effective. These include:
- Baricitinib (Olumiant)
- Tofacitinib (Xeljanz)
- Upadacitinib (Rinvoq)
Keep in mind that higher doses of tofacitinib can elevate the risk of blood clots in the lungs, serious heart-related events, and cancer. As always, consult with your healthcare provider to determine the most suitable treatment plan based on your individual needs and health status.
Therapeutic Approaches for Rheumatoid Arthritis
When managing rheumatoid arthritis (RA), a comprehensive approach involves not only medications but also various therapies to enhance joint function and improve daily life. Here are some therapeutic strategies:
- Physical and Occupational Therapy:
- Your doctor may recommend a physical therapist or an occupational therapist.
- Exercises: These professionals will teach you exercises to maintain joint flexibility.
- Adaptive Techniques: They’ll suggest new ways to perform daily tasks that are gentler on your joints. For instance, using your forearms to pick up objects can reduce strain.
- Assistive Devices: These devices help you avoid stressing painful joints. Examples include kitchen knives with hand grips to protect finger and wrist joints, as well as tools like buttonhooks to make dressing easier.
- Consider exploring catalogs and medical supply stores for additional ideas and specialized aids.
Remember that personalized guidance from healthcare professionals is essential to tailor these therapies to your specific needs and improve your quality of life while managing RA.
Surgical Options for Rheumatoid Arthritis
When medications fail to prevent or slow joint damage, surgical intervention becomes a consideration. Surgery aims to repair damaged joints, restore function, and alleviate pain. Here are the main surgical procedures for rheumatoid arthritis:
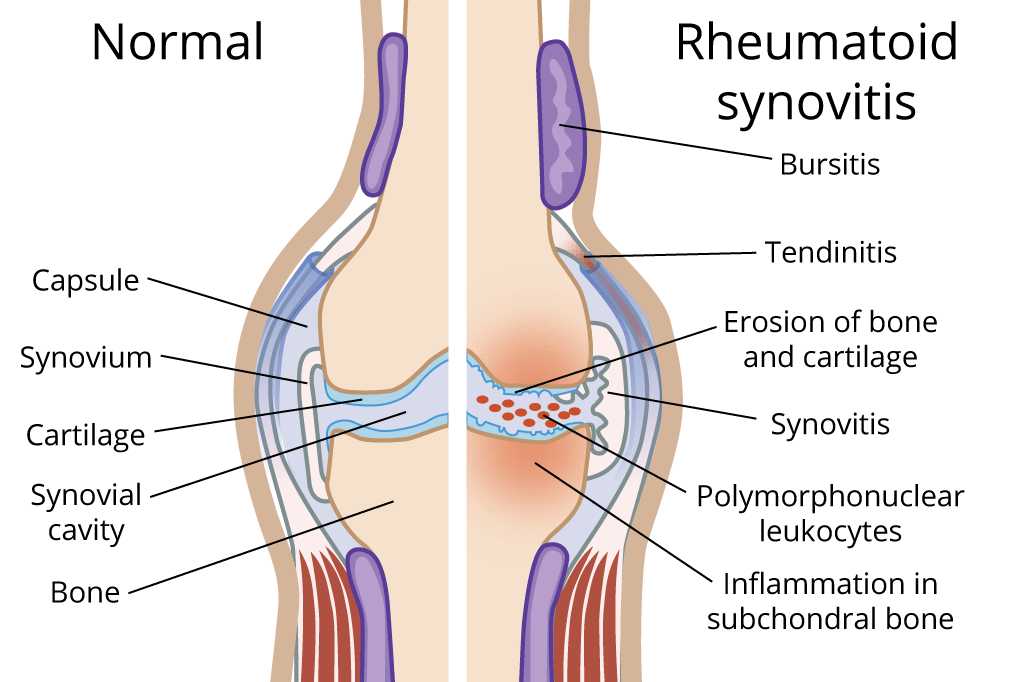
Synovectomy:
- This surgery involves removing the inflamed lining of the joint (synovium).
- It can help reduce pain and improve joint flexibility.
Tendon Repair:
- Inflammation and joint damage may cause tendons around the joint to loosen or rupture.
- Surgeons can repair these tendons to restore joint stability.
Joint Fusion (Arthrodesis):
- Joint fusion surgery stabilizes or realigns a joint.
- It provides pain relief when joint replacement is not feasible.
Total Joint Replacement (Arthroplasty):
- During joint replacement surgery, the surgeon removes damaged joint parts.
- A metal and plastic prosthesis is then inserted to replace the affected joint.
Remember that surgery carries risks such as bleeding, infection, and postoperative pain. It’s crucial to have an open discussion with your doctor about the potential benefits and risks based on your individual situation.
Lifestyle and Self-Care Strategies for Rheumatoid Arthritis
Taking proactive steps to care for your body can significantly improve your experience with rheumatoid arthritis (RA). These self-care measures, combined with your RA medications, can help manage symptoms effectively:
Regular Exercise:
- Engage in gentle exercises to strengthen the muscles around your joints.
- Exercise helps reduce fatigue and promotes overall well-being.
- Consult your doctor before starting any exercise regimen.
- If you’re a beginner, consider walking as a simple and effective option.
- Avoid exercising if you have tender, injured, or severely inflamed joints.
Heat and Cold Therapy:
- Heat: Apply heat to ease pain and relax tense muscles.
- Cold: Cold therapy can dull pain sensations and reduce swelling.
- Use these techniques as needed to manage discomfort.
Stress Reduction and Relaxation:
- Relaxation techniques can help you cope with pain and reduce stress.
- Consider practices such as guided imagery, deep breathing, and muscle relaxation.
- Managing stress contributes to better overall health.
Remember that personalized self-care, along with professional guidance, plays a crucial role in maintaining your quality of life while living with rheumatoid arthritis. Consult your healthcare provider for tailored advice and recommendations.
Alternative Approaches for Rheumatoid Arthritis
Complementary and alternative treatments can complement conventional therapies for rheumatoid arthritis (RA). Here are some promising options:
Fish Oil:
- Preliminary studies suggest that fish oil supplements may reduce RA pain and stiffness.
- Side effects can include nausea, belching, and a fishy taste in the mouth.
- Consult your doctor before using fish oil, especially if you’re taking other medications.
Plant Oils:
- Evening primrose, borage, and black currant seeds contain a type of fatty acid that may help with RA pain and morning stiffness.
- Side effects may include headache, diarrhea, and gas.
- Some plant oils can interfere with medications, so always check with your doctor first.
Tai Chi:
- Tai chi is a gentle movement therapy that combines exercises, stretches, and deep breathing.
- Many people use tai chi to reduce stress.
- Small studies indicate that tai chi may improve mood and quality of life in individuals with RA.
- When led by a knowledgeable instructor, tai chi is safe. Avoid moves that cause pain.
Remember to discuss these options with your healthcare provider to ensure they align with your overall treatment plan and health needs.
Coping Strategies for Rheumatoid Arthritis
Living with rheumatoid arthritis (RA) can be challenging, but there are ways to manage its impact on your daily life. Consider the following coping strategies:
Empowerment and Planning:
- Collaborate with your doctor to create a management plan for your arthritis.
- Feeling in control of your disease can positively influence your well-being.
Know Your Limits:
- Rest when fatigued. RA often leads to tiredness and muscle weakness.
- A short nap during the day (without affecting nighttime sleep) can be beneficial.
Connect with Others:
- Keep your family informed about your feelings and pain.
- Find a trusted family member or friend to talk to when you feel overwhelmed.
- Consider joining a support group for people with RA, either in your community or online.
Self-Care and Enjoyment:
- Prioritize self-care. Allocate time for activities you enjoy.
- Whether it’s writing in a journal, going for a walk, or listening to music, these moments can help reduce stress.
Remember that you’re not alone, and seeking support from loved ones and connecting with others who share similar experiences can make a significant difference in managing rheumatoid arthritis effectively.
Preparing for Your Rheumatoid Arthritis Appointment
Write Down:
- Detailed Descriptions of your symptoms.
- Medical History: Information about any past medical problems you’ve experienced.
- Family History: Details about medical issues affecting your parents or siblings.
- Medications and Supplements: List all current and past medications and dietary supplements related to this problem.
Anticipate Questions from Your Doctor:
- When did your symptoms begin?
- Have your symptoms changed over time?
- Which joints are affected?
- Does any activity improve or worsen your symptoms?
- Are your symptoms impacting daily tasks?
Remember to bring this information to your appointment, and feel free to ask any additional questions you may have. Your doctor will guide you through the evaluation process to determine the best course of action for managing your rheumatoid arthritis.