Anterior Vaginal Prolapse (Cystocele): A Comprehensive Guide
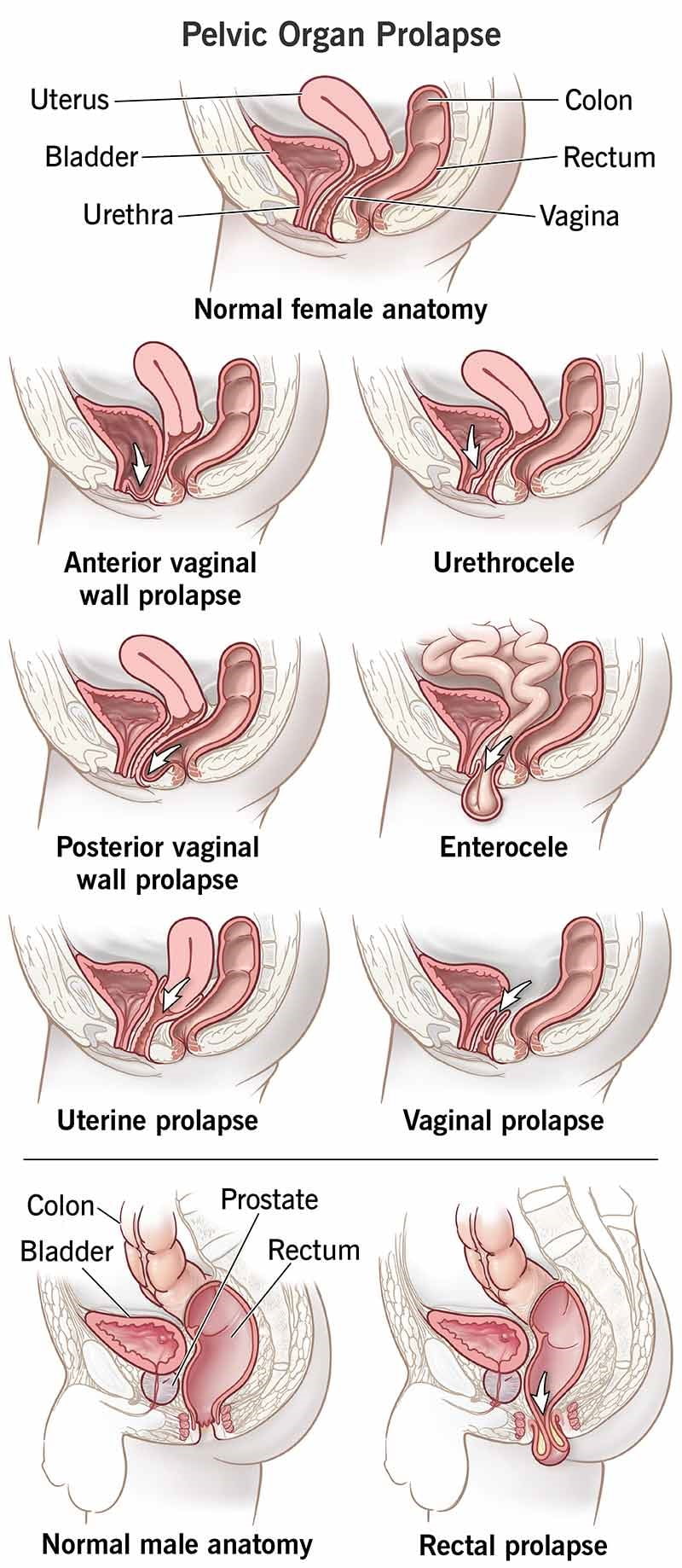
Understanding Anterior Vaginal Prolapse Commonly referred to as a cystocele or prolapsed bladder, anterior vaginal prolapse is a condition where the bladder descends from its normal position within the pelvis, exerting pressure against the vaginal wall.
This condition arises when the pelvic floor muscles and connective tissues—which support the bladder, uterus, and intestines—become weakened or overstretched. Factors contributing to this weakening include the natural aging process, the physical stress of vaginal childbirth, chronic constipation, persistent coughing, or regular heavy lifting.
Treatment Options Anterior vaginal prolapse can be managed effectively. Mild to moderate cases often respond well to non-surgical interventions. However, for more significant prolapses, surgical procedures may be required to maintain the correct positioning of the vagina and surrounding pelvic organs.
Recognizing Symptoms While minor prolapses may go unnoticed, more pronounced cases can present various symptoms, such as:
- A sensation of heaviness or pressure within the pelvis and vagina.
- Visible or palpable tissue protrusion within the vagina.
- Increased pelvic pressure during activities like straining, coughing, or lifting.
- Urinary issues, including difficulty initiating urination, incomplete bladder emptying, frequent urges to urinate, or urinary incontinence.
These symptoms are often more pronounced after prolonged standing and may subside upon lying down.
Consulting a Healthcare Professional Though a prolapsed bladder typically isn’t painful, it can lead to discomfort and complications like bladder infections. It’s advisable to seek medical advice if you experience any symptoms that disrupt your daily life.
Identifying Causes and Risk Factors The pelvic floor’s network of muscles, ligaments, and connective tissues provides support for your bladder and other pelvic organs. Over time, or due to specific traumas such as childbirth or chronic straining, these connections can weaken, leading to anterior prolapse.
Stressors that can impact the pelvic floor include:
- Pregnancy and vaginal childbirth.
- Excess body weight or obesity.
- Frequent heavy lifting.
- Constipation-related straining.
- Persistent coughing or conditions like bronchitis.
Risk Factors for Anterior Prolapse Certain conditions may elevate the likelihood of developing anterior prolapse:
- Pregnancy and Childbirth: Women with a history of vaginal or instrument-assisted deliveries, multiple births, or delivering large infants face a heightened risk.
- Aging: The risk escalates with age, particularly post-menopause, when estrogen levels—and consequently, pelvic floor strength—diminish.
- Hysterectomy: Uterus removal can potentially weaken the pelvic floor, though this isn’t universally the case.
- Genetic Predisposition: Inherent weaknesses in connective tissue may predispose some women to prolapse.
- Obesity: Higher body weight increases the risk of anterior prolapse.
If you’re preparing for a medical appointment regarding anterior prolapse, it’s beneficial to note any symptoms you’ve experienced, consider any relevant personal medical history, and be ready to discuss any concerns with your healthcare provider. This proactive approach can help ensure a comprehensive evaluation and effective treatment plan.
| Aspect | Details |
|---|---|
| Overview | A condition where the bladder descends and pushes against the vaginal wall due to weakened pelvic floor muscles. |
| Symptoms | Fullness or pressure in the pelvis, tissue bulge, urinary problems, symptoms worsen with standing and may improve when lying down. |
| When to See a Doctor | If symptoms are bothersome or affect daily activities, especially if leading to bladder infections. |
| Causes | Weakening of pelvic floor muscles and connective tissues due to aging, childbirth, heavy lifting, straining, or chronic coughing. |
| Risk Factors | Pregnancy, childbirth, aging, hysterectomy, genetics, obesity. |
| Diagnosis | Pelvic exam, questionnaire, bladder and urine tests. |
| Treatment | Non-surgical options like pelvic floor exercises and pessaries; surgical options for severe cases. |
| Lifestyle and Home Remedies | Kegel exercises, dietary changes, proper lifting techniques, cough management, weight management. |
| Preparing for Appointment | Document symptoms, medical history, bring a companion, prepare questions for the doctor. |
| Questions to Ask | Causes, tests needed, treatment options, risk of recurrence, activity restrictions, home symptom management, need for specialist. |
| Expectations from Doctor | Questions about symptoms onset, leakage, infections, pain during intercourse, coughing, constipation, family history, childbirth, future pregnancy plans. |