Diagnosing and Treating Anterior Vaginal Prolapse
Diagnosis Procedures The diagnosis of anterior vaginal prolapse typically includes:
- Pelvic Examination: This assessment is conducted both while you are lying down and standing. The healthcare provider will look for any protrusion of tissue into the vagina, indicative of a prolapse. You may be asked to bear down as if you are having a bowel movement to evaluate the extent of the prolapse. Additionally, you’ll perform a contraction of your pelvic floor muscles, akin to halting urination, to test their strength.
- Questionnaire: A detailed form will be provided for you to complete, which assists the healthcare provider in understanding your medical history, the severity of your prolapse, and its impact on your life. This information is crucial for determining the appropriate treatment path.
- Bladder Function Tests: Should your prolapse be substantial, tests may be conducted to ascertain the efficiency and completeness of your bladder emptying. Urine tests may also be performed to detect any bladder infections, particularly if urine retention is suspected.
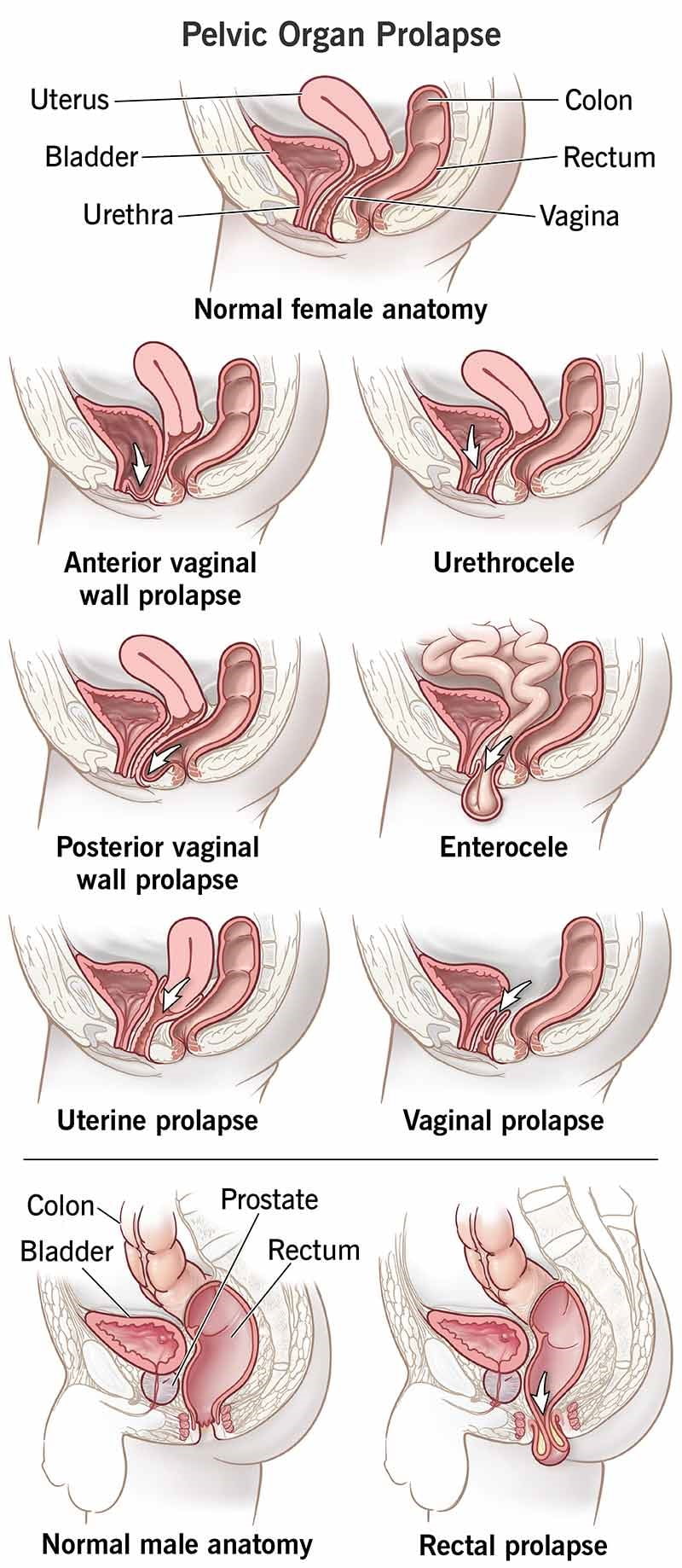
Treatment Approaches The treatment for anterior vaginal prolapse is contingent on the presence and intensity of symptoms, as well as any concurrent conditions like urinary incontinence or multiple pelvic organ prolapses.
- Mild Cases: In instances with minimal or no symptoms, treatment may not be necessary. A monitoring approach with periodic check-ups may be recommended.
- Symptomatic Cases: For those experiencing symptoms, initial treatments may include:
- Pelvic Floor Muscle Exercises: Commonly known as Kegel exercises, these are designed to fortify the pelvic floor muscles, thereby providing better support for the bladder and other organs. A healthcare provider or physical therapist can guide you through these exercises and ensure proper technique.
- Vaginal Pessary: This device, made of plastic or rubber, is inserted into the vagina to offer support to the bladder. While it doesn’t rectify the prolapse, it can alleviate symptoms. Healthcare professionals will fit and instruct you on its maintenance.
Surgical Intervention Surgery may be considered if symptoms persist despite non-surgical treatments.
- Procedure Details: Typically performed through the vagina, the surgery involves repositioning the prolapsed bladder and removing excess vaginal tissue. Tissue grafts may be utilized for additional support if the vaginal tissues are notably thin.
- Associated Prolapsed Uterus: In cases where a prolapsed uterus is present, a hysterectomy may be recommended alongside pelvic floor repair.
- Incontinence Issues: If stress incontinence is a factor, procedures to support the urethra may be suggested to alleviate symptoms.
- Pregnancy Considerations: Surgery may be postponed if pregnancy is planned or underway. Non-surgical options like pelvic exercises or a pessary can provide symptom relief in the interim. Although surgical benefits can be long-lasting, there is a risk of recurrence, potentially necessitating future surgery.
Home Management and Preparations for Anterior Vaginal Prolapse
Strengthening Your Pelvic Floor at Home Kegel exercises are a beneficial routine to enhance the strength of your pelvic floor muscles, offering improved support for your pelvic organs and mitigating symptoms linked to anterior prolapse.
Here’s how to execute Kegel exercises effectively:
- Engage your pelvic floor muscles, the same ones utilized to halt urination.
- Maintain the muscle contraction for five seconds, then relax for an equal duration. If challenging, begin with a two-second hold and a three-second relaxation period.
- Gradually increase to a ten-second hold.
- Aim for three sets of ten repetitions daily.
Consult with your healthcare provider for precise guidance on performing Kegels correctly and to confirm you’re engaging the appropriate muscles. Once mastered, Kegel exercises can be performed inconspicuously at any time, whether seated at work or lounging at home.
Lifestyle Adjustments to Prevent Prolapse Progression
- Dietary Changes: Incorporate high-fiber foods to prevent and manage constipation.
- Proper Lifting Techniques: Use your legs for lifting, not your waist or back, and avoid heavy lifting when possible.
- Cough Management: Seek treatment for persistent coughs or bronchitis, and avoid smoking.
- Weight Management: Discuss with your doctor to identify your ideal weight and explore weight-loss methods if necessary.
Preparing for Your Medical Consultation
If you’re experiencing symptoms of anterior prolapse that impact your daily life, schedule a visit with your primary care provider or gynecologist.
Pre-appointment Tips
- Document any symptoms you’ve experienced, including their duration.
- Compile a list of your medical history, current treatments, and any medications or supplements you’re taking.
- Consider bringing someone with you to the appointment to help remember information.
- Prepare a list of questions for your healthcare provider, prioritizing the most critical ones.
Essential Questions to Ask About Anterior Prolapse
- What could be causing my symptoms?
- Are there other potential causes?
- What tests are needed for a diagnosis?
- What are the treatment options?
- What are the next steps if the initial treatment isn’t effective?
- What are the risks of complications?
- What is the recurrence rate after treatment?
- Are there any restrictions I should follow?
- How can I alleviate symptoms at home?
- Is there a need to consult a specialist?
Expectations During the Consultation
Your healthcare provider may inquire about:
- The onset of your symptoms.
- Issues with urine leakage.
- Recurrence of bladder infections.
- Pain or urine leakage during sexual activity.
- Persistent or severe coughing.
- Constipation and straining during bowel movements.
- Factors that alleviate or exacerbate your symptoms.
- Family history of pelvic floor problems.
- History of vaginal childbirth and future pregnancy plans.
- Any additional concerns you may have.
Remember, it’s important to ask additional questions or seek clarifications during your appointment to ensure you fully understand your condition and the recommended management plan.
| Aspect | Details |
|---|---|
| Overview | A condition where the bladder descends and pushes against the vaginal wall due to weakened pelvic floor muscles. |
| Symptoms | Fullness or pressure in the pelvis, tissue bulge, urinary problems, symptoms worsen with standing and may improve when lying down. |
| When to See a Doctor | If symptoms are bothersome or affect daily activities, especially if leading to bladder infections. |
| Causes | Weakening of pelvic floor muscles and connective tissues due to aging, childbirth, heavy lifting, straining, or chronic coughing. |
| Risk Factors | Pregnancy, childbirth, aging, hysterectomy, genetics, obesity. |
| Diagnosis | Pelvic exam, questionnaire, bladder and urine tests. |
| Treatment | Non-surgical options like pelvic floor exercises and pessaries; surgical options for severe cases. |
| Lifestyle and Home Remedies | Kegel exercises, dietary changes, proper lifting techniques, cough management, weight management. |
| Preparing for Appointment | Document symptoms, medical history, bring a companion, prepare questions for the doctor. |
| Questions to Ask | Causes, tests needed, treatment options, risk of recurrence, activity restrictions, home symptom management, need for specialist. |
| Expectations from Doctor | Questions about symptoms onset, leakage, infections, pain during intercourse, coughing, constipation, family history, childbirth, future pregnancy plans. |