Diagnosing Angina: Tests and ProceduresInitial AssessmentA healthcare professional will begin by evaluating your symptoms and medical history, including any family history of heart disease, to diagnose angina.Diagnostic TestsElectrocardiogram (ECG or EKG)An ECG is a fundamental test that records the heart’s electrical activity using electrodes on the chest, arms, and legs. It can detect abnormal heart rhythms and signs of a heart attack.Chest X-rayA chest X-ray provides images of the heart and lungs, helping to rule out other causes of chest pain and check for an enlarged heart.Blood TestsBlood tests look for cardiac enzymes that indicate heart damage, such as from a heart attack.Stress TestA stress test involves exercising on a treadmill or stationary bike to make diagnosing angina easier when the heart is more active. Medications may be used to simulate exercise effects if physical activity isn’t possible.EchocardiogramAn echocardiogram uses ultrasound waves to create moving images of the heart, showing blood flow and heart function.Nuclear Stress TestIn a nuclear stress test, a radioactive tracer is injected to visualize blood flow to the heart muscle during rest and stress, identifying areas with poor circulation.Cardiac CT and MRICardiac CT and MRI scans generate detailed images of the heart and chest, revealing the extent of heart damage.Coronary AngiogramA coronary angiogram involves inserting a catheter into a blood vessel to guide dye to the heart, allowing X-ray imaging of the heart’s blood vessels during cardiac catheterization.These tests collectively help healthcare professionals confirm the presence of angina and understand its severity, guiding appropriate treatment strategies.
Angina Treatment: A Comprehensive Approach
Lifestyle Modifications
To manage angina, the following lifestyle changes are recommended:Healthy diet: Emphasize a balanced diet rich in fruits, vegetables, and whole grains.
Regular exercise: Engage in physical activity that suits your fitness level and health status.
Medical Interventions
When lifestyle adjustments are insufficient, medical treatments may include:
Medications: Such as nitrates, aspirin, clot-preventing drugs, beta blockers, statins, calcium channel blockers, and other blood pressure medications.
Angioplasty and stenting: To open narrowed arteries and improve blood flow.
Coronary artery bypass grafting (CABG): Open-heart surgery to bypass blocked arteries.
Treatment Goals
The primary objectives of angina treatment are to:
Reduce frequency of angina episodes.
Alleviate severity of symptoms.
Decrease risk of heart attack and death.
Medication Details
Nitrates
Function: Relax and widen blood vessels, increasing blood flow to the heart.
Common Form: Nitroglycerin (Nitrostat), typically placed under the tongue.
Usage: Before activities that trigger angina or on a long-term basis for prevention.
Aspirin
Function: Reduces blood clotting, facilitating blood flow through narrowed arteries.
Note: Consult with your healthcare team before starting a daily aspirin regimen.
Clot-Preventing Drugs
Examples: Clopidogrel (Plavix), prasugrel (Effient), ticagrelor (Brilinta).
Function: Prevent blood platelets from clumping together, reducing clot formation.
Beta Blockers
Function: Slow the heartbeat and lower blood pressure, improving blood flow.
Statins
Function: Lower blood cholesterol by blocking a substance needed for cholesterol production.
Calcium Channel Blockers
Function: Relax and widen blood vessels, enhancing blood flow.
Other Blood Pressure Medications
Examples: ACE inhibitors and ARBs.
Indications: For patients with high blood pressure, diabetes, heart failure, or kidney disease.
Ranolazine
Use: For chronic stable angina not responsive to other medications.
Immediate treatment is crucial for unstable angina or chest pain that deviates from your usual pattern. Always consult with your healthcare team for personalized advice and treatment plans.
Therapies and Management for Angina
Non-Drug Therapies
Enhanced External Counterpulsation (EECP): A treatment that involves cuffs around the calves, thighs, and pelvis to boost blood flow to the heart. It’s beneficial for refractory angina.
Surgical and Procedural Interventions
When other treatments fail to alleviate angina, the following procedures may be considered:
Angioplasty with Stenting
Also Known As: Percutaneous coronary intervention.
Procedure: A balloon is inserted and inflated in the narrowed artery, followed by a stent to keep it open.
Benefits: Improves blood flow and can reduce or eliminate angina, suitable for unstable angina or chronic stable angina unresponsive to other treatments.
Coronary Artery Bypass Grafting (CABG)
Type: Open-heart surgery.
Procedure: A vein or artery is grafted to bypass a blocked heart artery.
Indications: For both unstable angina and stable angina not improved by other methods.
Lifestyle and Home Remedies
Lifestyle modifications play a crucial role in managing angina and heart health:
Quit Smoking: The single most beneficial action for heart health.
Regular Exercise: Aim for at least 30 minutes of activity most days of the week.
Weight Management: Maintain a healthy weight to reduce strain on the heart.
Healthy Diet: Opt for a diet low in saturated fat, trans fats, salt, and sugar, and rich in whole grains, fruits, vegetables, and lean proteins.
Manage Health Conditions: Regularly monitor blood pressure, blood sugar, and cholesterol levels.
Stress Control: Engage in stress-reducing activities like exercise, mindfulness, and support groups.
Moderate Alcohol Consumption: Limit intake to one drink per day for women and two for men.
Good Sleep Habits: Aim for 7 to 9 hours of sleep daily and maintain consistent sleep routines.
These strategies are integral to preventing angina and promoting overall cardiovascular health. Always consult with your healthcare team for personalized advice and treatment plans.
Preparing for Your Angina Appointment: A GuideBefore the Appointment
Understand Restrictions: Confirm if you need to fast or avoid certain activities before tests.
Document Symptoms: Record any symptoms, their onset, and activities during their occurrence.
Personal and Family History: Note down any personal or family history of heart-related issues and other health conditions.
Medication List: Compile a list of all medications, vitamins, and supplements you’re taking, including dosages.
Bring Support: Consider having someone accompany you to help remember the discussion.
Questions for Your Healthcare Team
Causes: What could be causing my chest pain?
Tests Needed: Which tests will I undergo, and how should I prepare?
Treatment Recommendations: What treatments do you suggest, and what are their benefits?
Physical Activity: What type and amount of exercise is safe for me?
Managing Other Conditions: How can I best manage my angina alongside other health issues?
Follow-Up: How frequently should I check in about my angina?
Resources: Can you provide any brochures or recommend informative websites?
Expectations During the Visit
Symptom Discussion: Be prepared to describe your chest pain and any related symptoms in detail.
Medical History Review: Your doctor will inquire about the history and pattern of your symptoms.
Lifestyle Inquiry: Expect questions about your diet, exercise habits, and stress levels.
In the Meantime
Lifestyle Changes: Start making heart-healthy lifestyle adjustments to reduce the risk of angina complications.
Remember, this appointment is an opportunity to address your concerns and understand your condition better. Don’t hesitate to ask questions and seek clarity on any aspect of your health.
Category | Details |
|---|---|
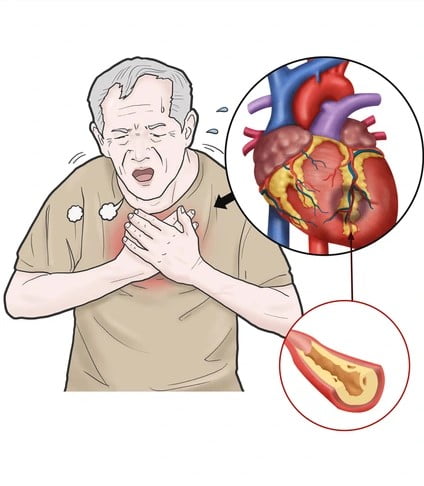
Understanding Angina | Angina, also known as angina pectoris, is chest pain due to reduced blood flow to the heart, indicating coronary artery disease. |
Types of Angina | Stable angina, unstable angina, variant angina (Prinzmetal angina), and refractory angina. |
Symptoms of Angina | Chest pain, discomfort, burning, fullness, pressure, squeezing, dizziness, fatigue, nausea, shortness of breath, sweating. |
Angina in Women | Symptoms may differ, such as discomfort in the neck, jaw, teeth, back, nausea, shortness of breath, stabbing pain, and stomach pain. |
Risk Factors | Age, family history, tobacco use, diabetes, high blood pressure, high cholesterol/triglycerides, other health conditions, lack of exercise, obesity, emotional stress, certain medications, drug misuse, cold temperatures. |
Complications | The most severe complication is a heart attack, with symptoms like chest pressure, pain extending beyond the chest, fainting, a sense of doom, increasing episodes of chest pain, nausea, vomiting, upper belly pain, shortness of breath, sweating. |
Prevention | Lifestyle changes such as avoiding alcohol, not smoking, eating healthily, exercising, maintaining a healthy weight, managing health conditions, reducing stress, getting enough sleep, and vaccinations. |
Diagnosis | Through patient examination, ECG, chest X-ray, blood tests, stress test, echocardiogram, nuclear stress test, cardiac CT/MRI, coronary angiogram. |
Treatment | Lifestyle changes, medications (nitrates, aspirin, clot-preventing drugs, beta blockers, statins, calcium channel blockers, other blood pressure medicines, ranolazine), angioplasty with stenting, coronary artery bypass grafting (CABG). |
Therapies | Enhanced external counterpulsation (EECP) for refractory angina. |
Surgery and Procedures | Angioplasty with stenting, coronary artery bypass grafting (CABG). |
Lifestyle and Home Remedies | Quit smoking, regular exercise, manage weight, eat a healthy diet, manage other health conditions, control stress, limit alcohol, practice good sleep habits. |
Preparing for Appointment | Understand pre-appointment restrictions, document symptoms, note personal and family history, list all medications, bring support, be prepared to discuss diet and exercise, write down questions. |