Diagnosing Anal Fistulas
Initial Consultation and Physical Examination
Diagnosis begins with a healthcare provider discussing symptoms and conducting a physical examination, which includes inspecting both the external and internal areas around the anus.
Identifying the Fistula
The external opening of an anal fistula is typically visible on the skin, while locating the internal opening within the anal canal is more challenging. A comprehensive understanding of the fistula’s pathway is crucial for effective treatment.
Imaging Tests for Fistula Detection
A variety of imaging tests may be employed to trace the fistula tunnel:
- Magnetic Resonance Imaging (MRI): This technique maps the fistula tunnel and captures intricate images of the sphincter muscle and pelvic floor structures.
- Endoscopic Ultrasound: Utilizing high-frequency sound waves, this test can pinpoint the fistula, the sphincter muscles, and adjacent tissues.
- Fistulography: An X-ray procedure that injects contrast to visualize the anal fistula tunnel.
Examination Under Anesthesia
For a comprehensive assessment, a colon and rectal surgeon may perform an examination under anesthesia, allowing for an in-depth evaluation of the fistula tunnel and the identification of any complications.
Additional Diagnostic Tools
Other methods to locate the fistula’s internal opening include:
- Fistula Probe: A specialized instrument inserted through the fistula to delineate the tunnel.
- Anoscope: A diminutive endoscope for examining the anal canal.
- Flexible Sigmoidoscopy or Colonoscopy: These endoscopic procedures inspect the large intestine. Sigmoidoscopy assesses the sigmoid colon, while colonoscopy, which reviews the entire colon, is vital for detecting other conditions, particularly if ulcerative colitis or Crohn’s disease is suspected.
- Injected Dye Solution: This can assist in identifying the fistula’s internal opening.
Treatment Approaches for Anal Fistulas
Treatment Objectives
The primary goals in treating an anal fistula are to completely heal the fistula, prevent its recurrence, and safeguard the sphincter muscles to avoid fecal incontinence. While surgery is the standard treatment, there are cases where nonsurgical options may be viable.
Surgical Treatments
Fistulotomy
This procedure involves the surgeon making an incision at the fistula’s internal opening, cleaning out the infected area, and then suturing the flattened tunnel. Complex fistulas might require a staged fistulotomy, especially if a significant portion of the sphincter muscle is involved or the entire tunnel is not identifiable.
Endorectal Advancement Flap
The surgeon constructs a flap from the rectal wall to cover the fistula’s internal opening after its removal. This technique aims to minimize the cutting of sphincter muscle.
Ligation of the Intersphincteric Fistula Tract (LIFT)
The LIFT procedure is a two-stage approach for treating complex or deep fistulas. It involves placing a seton to gradually dilate the tunnel, followed by the removal of infected tissue and closure of the internal opening, all while preserving the sphincter muscles.
Nonsurgical Options
Seton Placement
A seton is placed within the fistula to facilitate drainage and healing, sometimes in conjunction with surgical procedures.
Fibrin Glue and Collagen Plug
After cleaning the tunnel and closing the internal opening, a fibrin-based adhesive or a collagen plug is used to seal the external opening of the fistula.
Medication
Medications are considered when Crohn’s disease is identified as the underlying cause of the anal fistula.
Procedures for Complex Cases
Ostomy and Stoma
For intricate fistulas, a temporary abdominal opening may be created to divert intestinal contents, allowing the anal region to recover.
Muscle Flap
In cases of extremely complex fistulas, the tunnel may be filled with healthy muscle tissue sourced from the thigh, labia, or buttock.
Managing Anal Fistula at Home
Comfort Measures During Healing
To alleviate discomfort during the healing process, consider the following suggestions from your healthcare provider:
- Pain Management: Use over-the-counter or prescribed pain medication as needed.
- Warm Sitz Baths: Soak in a warm bath to soothe the affected area.
- Dietary Adjustments: Increase fiber intake and consume ample fluids to avoid constipation.
- Bowel Movement Care: Refrain from straining during bowel movements to prevent aggravation.
Preparing for Your Medical Appointment
Referral to Specialists
For anal fistula concerns, you may be directed to a gastroenterologist or a colon and rectal surgeon for specialized care.
Pre-Appointment Checklist
Prior to your appointment, consider the following preparatory steps:
- Fasting: Confirm if fasting is required before undergoing certain tests.
- Symptom Record: Compile a list of all symptoms, regardless of their apparent relevance.
- Personal Information: Gather details about personal stressors, life changes, and family medical history.
- Medication Inventory: List all medications, supplements, and their dosages that you’re currently taking.
Questions for Your Healthcare Provider
Prepare a set of questions to gain a better understanding of your condition, such as:
- What could be the root cause of my symptoms?
- Are there other potential causes?
- Are any tests necessary?
- Is this condition temporary or chronic?
- Can you recommend any dietary modifications?
- Should I adhere to any specific restrictions?
- What treatment options are available?
- Are there alternative treatments to consider?
- How should I manage this alongside my other health conditions?
- Can you provide any informational materials or recommend informative websites?
During the Appointment
Feel empowered to ask additional questions that arise during your consultation.
Queries from Your Healthcare Provider
Be prepared to answer questions from your doctor, including:
- When did you first notice your symptoms?
- Are your symptoms persistent or intermittent?
- How would you describe the severity of your symptoms?
- Where do you experience symptoms most intensely?
- Have you found anything that alleviates your symptoms?
- Is there anything that exacerbates your symptoms?
- Do you have any other health issues, like Crohn’s disease?
- Do you experience constipation?
| Section | Subsection | Details |
|---|---|---|
| Anal Fistula Overview | Formation | Abnormal tunnel from an infected anal gland to the skin. |
| Treatment Necessity | Surgical intervention is standard; nonsurgical options may apply. | |
| Symptoms | Common Indicators | Discharge, pain, fever, and inflammation around the anus. |
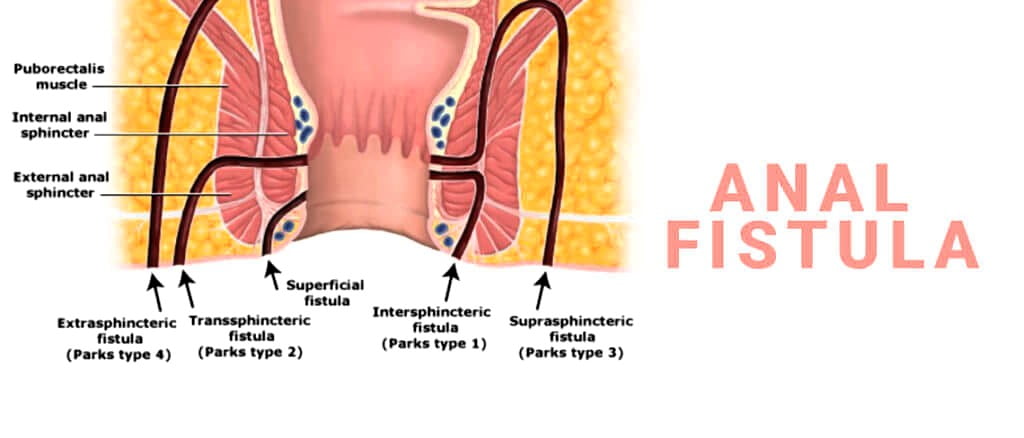
| Causes | Origin | Infection in an anal gland leading to an abscess and fistula formation. |
| Sphincter Muscle Involvement | Classification based on sphincter muscle involvement aids treatment planning. | |
| Risk Factors | Common Risks | History of abscesses, inflammatory bowel diseases, trauma, infections, and anal cancer treatments. |
| Demographics | More common in adults around 40, especially males and those with Crohn’s disease. | |
| Complications | Recurrence and Incontinence | Possibility of recurrence and fecal incontinence post-treatment. |
| Diagnosis | Physical Exam | Inspection of the external and internal anal area. |
| Imaging Tests | MRI, endoscopic ultrasound, fistulography, and examination under anesthesia. | |
| Additional Tools | Fistula probe, anoscope, sigmoidoscopy/colonoscopy, and injected dye solution. | |
| Treatment | Surgical Options | Fistulotomy, endorectal advancement flap, LIFT, ostomy and stoma, muscle flap. |
| Nonsurgical Options | Seton placement, fibrin glue and collagen plug, medication for Crohn’s disease. | |
| Lifestyle and Home Remedies | Comfort Measures | Pain medication, warm sitz baths, dietary fiber, and avoiding straining. |
| Preparing for Appointment | Specialist Referral | Gastroenterologist or colon and rectal surgeon. |
| Pre-Appointment | Fasting instructions, symptom record, personal information, medication inventory. | |
| Questions for Provider | Causes, tests, condition duration, dietary suggestions, treatment recommendations. | |
| Doctor’s Questions | Symptom onset, severity, location, improvement/worsening factors, other medical conditions. |