Diagnosing achalasia involves a thorough evaluation to differentiate it from other digestive disorders. Your doctor may recommend the following tests:
Esophageal Manometry: This test assesses rhythmic muscle contractions in your esophagus during swallowing. It measures the coordination and force exerted by the esophageal muscles. Additionally, it evaluates how well your lower esophageal sphincter relaxes or opens during swallowing. Esophageal manometry is particularly useful in identifying the type of motility problem you might have.
X-rays of the Upper Digestive System (Esophagram): After consuming a chalky liquid, X-rays are taken to visualize the inside lining of your digestive tract. This allows your doctor to observe a silhouette of your esophagus, stomach, and upper intestine. Sometimes, you may be asked to swallow a barium pill to highlight any blockage in the esophagus.
Upper Endoscopy: During this procedure, a thin, flexible tube equipped with a light and camera (endoscope) is inserted down your throat. The endoscope allows your doctor to examine the interior of your esophagus and stomach. It can help define partial blockages in the esophagus based on symptoms or barium study results. Additionally, endoscopy enables the collection of tissue samples (biopsy) for testing complications related to reflux, such as Barrett’s esophagus.
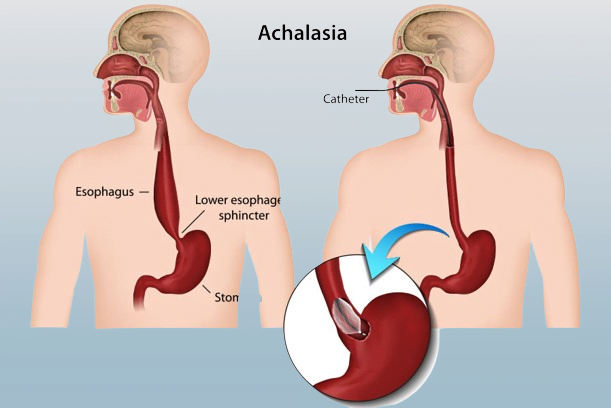
Achalasia, a condition where food and liquid struggle to pass through the esophagus into the stomach, can be managed through various treatments. Here are the options:
- Nonsurgical Treatments:
- Pneumatic Dilation: During this outpatient procedure, a balloon is inserted into the esophageal sphincter and inflated to widen the opening. If necessary, it may need to be repeated within approximately six years.
- Botox Injections: Botulinum toxin type A (Botox) can be directly injected into the esophageal sphincter using an endoscopic needle. Repeat injections may be required, but they should not hinder future surgery. Botox effects typically last up to six months and can help confirm an achalasia diagnosis.
- Medication: Muscle relaxants like nitroglycerin or nifedipine may be recommended before meals.
Remember that the choice of treatment depends on individual factors such as age, health status, and the severity of achalasia. Consult with your healthcare provider to determine the most suitable approach for you.
Treatment Options for Achalasia:
Medication:
- Your doctor may recommend muscle relaxants such as nitroglycerin (Nitrostat) or nifedipine (Procardia) before meals. However, these medications have limited effectiveness and may cause severe side effects.
- Medications are typically considered when patients are not suitable candidates for pneumatic dilation or surgery and if Botox injections haven’t been effective. This type of therapy is rarely used.
Surgical Approaches:
- Heller Myotomy: In this procedure, the surgeon cuts the muscle at the lower end of the esophageal sphincter. This allows food to pass more easily into the stomach. Heller myotomy can be performed noninvasively using laparoscopy.
- To prevent future issues with gastroesophageal reflux disease (GERD), a simultaneous procedure called fundoplication may be done during Heller myotomy. Fundoplication involves wrapping the top of the stomach around the lower esophagus to create an anti-reflux valve, preventing acid from flowing back into the esophagus.
- Peroral Endoscopic Myotomy (POEM): In POEM, an endoscope is inserted through the mouth and down the throat to create an incision in the esophageal lining. Similar to Heller myotomy, the surgeon cuts the muscle at the lower end of the esophageal sphincter.
- POEM may be followed by fundoplication to reduce the risk of GERD. Some patients who develop GERD after POEM receive daily oral medication .