Diagnosing Anthrax
To determine the likelihood of anthrax exposure, your doctor will inquire about your occupation and other relevant factors. Initially, common conditions with similar symptoms, such as the flu or pneumonia, will be ruled out.
Diagnostic Tests for Anthrax
If anthrax infection is suspected, the following tests may be conducted:
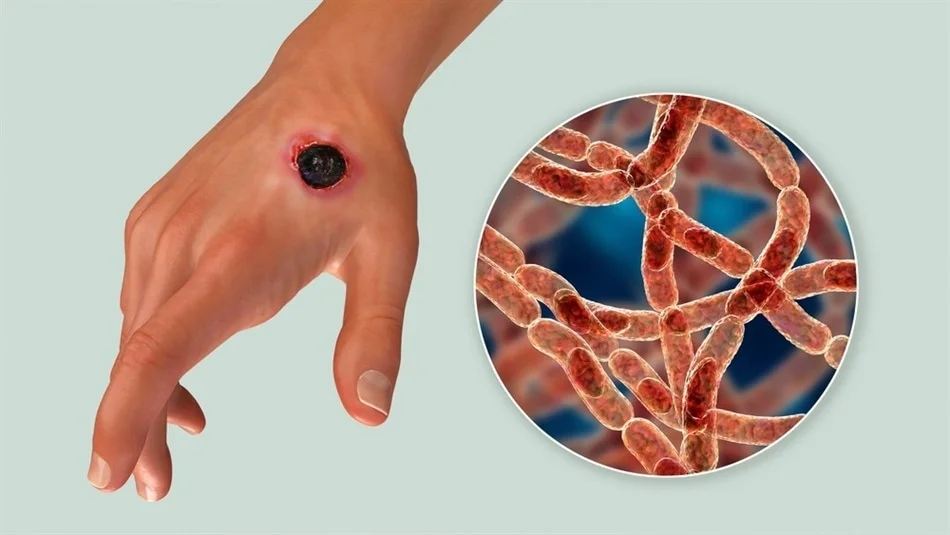
Skin Testing: Fluid from skin lesions or tissue samples may be analyzed for cutaneous anthrax indicators.
Blood Tests: Blood samples are examined for the presence of anthrax bacteria.
Imaging: A chest X-ray or CT scan may be utilized to diagnose inhalation anthrax.
Stool Testing: Stool samples can be tested for gastrointestinal anthrax.
Spinal Tap (Lumbar Puncture): This procedure, involving the extraction of spinal fluid, is recommended when systemic anthrax is suspected to check for meningitis.
Anthrax Treatment
The primary treatment for anthrax involves antibiotics and, in certain cases, antitoxins. The choice of antibiotics is tailored based on the infection’s specifics, including the number of people affected, the anthrax strain, and individual health factors. Early initiation of treatment is crucial for effectiveness.
Post-2001 bioterrorism events, antitoxin therapies like raxibacumab and obiltoxaximab have been developed for inhalation anthrax to target the toxins produced by the bacteria. Anthrax immunoglobulin may also be used for toxin neutralization. These are supplementary to antibiotics and accessible via the U.S. Centers for Disease Control and Prevention.
Injection anthrax has been treated successfully with surgical removal of infected tissues. However, advanced inhalation anthrax may not respond to antibiotics alone due to excessive toxin production.
Supportive care for anthrax may include ventilators, fluids, and vasopressors to manage blood pressure.
Preparing for a Medical Appointment
If exposed to anthrax or experiencing symptoms, immediate emergency care is necessary. Prior to visiting the ER:
Document symptoms: Note all symptoms, even if they seem unrelated to anthrax.
Record personal information: Recent travel to endemic areas, exposure to animals or animal products, etc.
List medications: Include all medicines, vitamins, and supplements.
Bring someone along: A companion can help remember details from the appointment.
Prepare questions: Ask about the infection route, treatment options, and prognosis if diagnosed with anthrax.
Category | Details |
|---|---|
Overview | A rare but serious bacterial disease, primarily affecting livestock and occasionally humans. |
Transmission | Direct or indirect contact with infected animals; not typically transmissible between humans. |
Symptoms | Varies by infection type; can include skin sores, vomiting, shock, and more. |
Types of Anthrax | Cutaneous, Inhalation, Gastrointestinal, Injection. |
Cutaneous Anthrax | Most common; symptoms include itchy bumps, sores with black centers, swelling, fever. |
Gastrointestinal | From eating contaminated meat; symptoms include nausea, abdominal pain, bloody diarrhea. |
Inhalation Anthrax | From inhaling spores; severe and often fatal, with symptoms like fever, chest discomfort. |
Injection Anthrax | Linked to injecting drugs; symptoms include redness, swelling at the injection site. |
Risk Factors | Military, lab workers, handling animal products, veterinary work, illegal drug use. |
Complications | Sepsis, hemorrhagic meningitis. |
Prevention | Vaccines, avoiding contact with infected animals, proper cooking of meat. |
Diagnosis | Based on exposure risk, symptoms; confirmed via skin testing, blood tests, imaging, stool tests. |
Treatment | Antibiotics, antitoxins, supportive care; early treatment is critical. |
When to See a Doctor | If exposed or symptoms develop after contact with animals in endemic areas. |
Causes | Anthrax spores in soil; dormant until entering a host like livestock. |
Public Health Concerns | Rare in developed countries; used in bioterrorism, linked to drug use in Europe. |