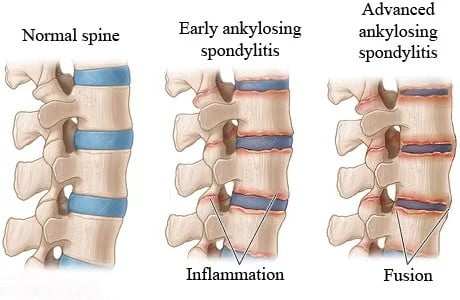
Ankylosing spondylitis, also known as axial spondyloarthritis, is an inflammatory disease that gradually causes some of the vertebrae (bones in the spine) to fuse. This fusion reduces spinal flexibility and can lead to a hunched posture. When the ribs are affected, it may become challenging to breathe deeply.
There are two types of axial spondyloarthritis:
Ankylosing spondylitis: This type is visible on X-rays and is characterized by fusion of the vertebrae.
Nonradiographic axial spondyloarthritis: Although not visible on X-rays, this type is diagnosed based on symptoms, blood tests, and other imaging techniques.
Symptoms typically begin in early adulthood. Inflammation can also occur in other parts of the body, most commonly affecting the eyes.
While there is no cure for ankylosing spondylitis, treatments can help manage symptoms and potentially slow disease progression.
Commonly affected areas include:
The joint between the base of the spine and the pelvis.
The vertebrae in the lower back.
The points where tendons and ligaments attach to bones, primarily in the spine (and occasionally along the back of the heel).
The cartilage between the breastbone and the ribs.
The hip and shoulder joints.
Ankylosing Spondylitis: A Closer Look
Overview Ankylosing spondylitis, also known as axial spondyloarthritis, is an inflammatory disease that gradually leads to the fusion of certain vertebrae (bones in the spine). As these vertebrae fuse, the spine becomes less flexible, potentially resulting in a hunched posture. Additionally, if the ribs are affected, breathing deeply can become challenging.
There are two main types of axial spondyloarthritis:
Ankylosing spondylitis: This type is visible on X-rays and is characterized by the fusion of vertebrae.
Nonradiographic axial spondyloarthritis: Although not detectable on X-rays, this type is diagnosed based on symptoms, blood tests, and other imaging techniques.
Symptoms
Early symptoms often include back pain and stiffness in the lower back and hips, especially in the morning or after periods of inactivity.
Neck pain and fatigue are also common.
Over time, symptoms may worsen, improve, or occur at irregular intervals.
Commonly Affected Areas
The joint between the base of the spine and the pelvis.
The vertebrae in the lower back.
Points where tendons and ligaments attach to bones, primarily in the spine (and occasionally along the back of the heel).
The cartilage between the breastbone and the ribs.
The hip and shoulder joints.
When to Seek Medical Attention
If you experience low back or buttock pain that develops slowly, worsens in the morning, or disrupts your sleep in the second half of the night, consider seeking medical advice.
Eye symptoms (such as painful red eyes, severe light sensitivity, or blurred vision) require immediate evaluation by an eye specialist.
Causes and Risk Factors
The specific cause of ankylosing spondylitis remains unknown, but genetic factors play a role.
Individuals with the HLA-B27 gene are at a significantly higher risk of developing this condition. However, not everyone with the gene develops ankylosing spondylitis.
Complications
Spinal Fusion: In severe cases, new bone forms as part of the body’s healing response. This gradually bridges the gap between vertebrae, leading to stiffness and inflexibility.
Rib Cage Stiffening: Fusion can also affect the rib cage, limiting lung capacity and function.
Eye Inflammation (Uveitis): Uveitis is a common complication, causing rapid-onset eye pain, light sensitivity, and blurred vision.
Compression Fractures: Weakened vertebrae during early stages can result in a stooped posture and may put pressure on the spinal cord and nerves.
Heart Problems: Ankylosing spondylitis increases the risk of heart disease due to inflammation affecting the aorta and aortic valve.
Remember to consult a healthcare provider for personalized advice and management strategies. 😊
Topic | Summary |
|---|---|
Overview | Ankylosing spondylitis (also known as axial spondyloarthritis) is an inflammatory disease that causes the fusion of vertebrae in the spine over time. This fusion reduces spinal flexibility and can lead to a hunched posture. If ribs are affected, breathing deeply becomes difficult. |
Types | – Ankylosing spondylitis: Visible on X-rays, characterized by vertebrae fusion. – Nonradiographic axial spondyloarthritis: Diagnosed based on symptoms, blood tests, and imaging. |
Symptoms | – Back pain and stiffness, especially in the morning or after inactivity. – Neck pain and fatigue. – Symptoms may worsen, improve, or occur irregularly. |
Commonly Affected Areas | – Joint between the base of the spine and the pelvis. – Vertebrae in the lower back. – Points where tendons and ligaments attach to bones (spine and back of the heel). – Cartilage between the breastbone and ribs. – Hip and shoulder joints. |
Diagnosis | – Physical exam assessing range of motion and pain. – X-rays (visible signs may not appear early). – MRI for nonradiographic cases. – No specific lab tests; HLA-B27 gene testing. |
Treatment | – Medications (NSAIDs, TNF blockers, IL-17 inhibitors, JAK inhibitors). – Physical therapy. – Surgery (if severe pain or hip joint damage). |
Self-Care | – Stay active. – Quit smoking. – Practice good posture. |
Coping and Support | – Understand condition variability. – Consider joining support groups. |
Preparing for Appointment | – Compile symptom details, personal information, and medication list. – Prepare questions for your doctor. |