Diagnosis of Ankylosing Spondylitis
Physical Examination:
During the physical exam, your healthcare provider will assess your spine’s range of motion.
They may ask you to bend in different directions and observe any pain or stiffness.
Specific portions of your pelvis may be pressed to reproduce pain, and leg movements may be manipulated to evaluate discomfort.
Breathing deeply will help determine chest expansion.
Imaging Tests:
X-rays: These allow doctors to check for changes in joints and bones. However, visible signs of ankylosing spondylitis (also known as axial spondyloarthritis) might not be evident early in the disease.
Magnetic Resonance Imaging (MRI): MRI scans provide more detailed images of bones and soft tissues. They can reveal evidence of nonradiographic axial spondyloarthritis earlier in the disease process, although they are more expensive.
Lab Tests:
There are no specific lab tests to diagnose ankylosing spondylitis.
Certain blood tests can check for markers of inflammation, but inflammation can result from various health conditions.
HLA-B27 Gene Testing:
Blood tests can detect the presence of the HLA-B27 gene.
However, it’s important to note that having the gene doesn’t necessarily mean an individual will develop ankylosing spondylitis, and some people with the disease don’t have this gene.
Treatment Options
Medications:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Commonly used to treat axial spondyloarthritis and nonradiographic axial spondyloarthritis.
Examples include naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB).
These medications relieve inflammation, pain, and stiffness but may cause gastrointestinal bleeding.
If NSAIDs are ineffective:
Tumor Necrosis Factor (TNF) Blockers or Interleukin-17 (IL-17) Inhibitors:
Administered via injection under the skin or through an intravenous line.
Janus Kinase (JAK) Inhibitors:
Taken orally.
Note: These medications can reactivate untreated tuberculosis and increase susceptibility to infections.
Physical Therapy:
An essential part of treatment.
Benefits include pain relief, improved strength, and enhanced flexibility.
A physical therapist can design specific exercises tailored to your needs:
Range-of-motion and stretching exercises.
Strengthening exercises for abdominal and back muscles.
Guidance on proper sleeping and walking positions to maintain good posture.
Surgery:
Most individuals with ankylosing spondylitis or nonradiographic axial spondyloarthritis do not require surgery.
Surgical intervention may be considered if:
Severe pain persists.
A hip joint is significantly damaged and needs replacement.
Self-Care Strategies for Ankylosing Spondylitis
Stay Active:
Regular exercise can help:
Ease pain.
Maintain flexibility.
Improve posture.
Consider low-impact activities such as swimming, walking, or gentle yoga.
Quit Smoking:
Smoking exacerbates health issues, including breathing difficulties.
If you smoke, take steps to quit.
Practice Good Posture:
Stand in front of a mirror and focus on maintaining proper posture.
Good posture can help prevent some of the problems associated with ankylosing spondylitis.
Coping and Support
Condition Variability:
Understand that the course of ankylosing spondylitis can change over time.
You may experience painful episodes interspersed with periods of less pain.
Despite the diagnosis, most people can lead productive lives.
Support Groups:
Consider joining an online or in-person support group for individuals with ankylosing spondylitis.
Sharing experiences and receiving support from others who understand your condition can be valuable.
Preparing for Your Medical Appointment
Compile Information:
Make a list of:
Your symptoms (including unrelated ones).
Major life stresses and recent changes.
Family medical history.
All medications, vitamins, and supplements you take.
Questions to Ask:
Bring a family member or friend along to help remember information.
Basic questions to ask your healthcare team:
What is likely causing my symptoms?
Are there other possible causes besides the most likely one?
What tests do I need?
Is my condition temporary or lifelong?
What treatment approach is best?
Are there alternative treatments?
How can I manage other health conditions alongside ankylosing spondylitis?
Are there specific restrictions I should follow?
Should I see a specialist?
Are there any helpful brochures or recommended websites?
Expectations from Your Doctor:
Your doctor will likely inquire about:
The location and severity of your pain.
Whether your symptoms are continuous or occasional.
Factors that worsen or improve your symptoms.
Any pain-relieving medications you’ve tried and their effectiveness.
Remember to consult your healthcare provider for personalized advice and tailored management strategies. 😊
Topic | Summary |
|---|---|
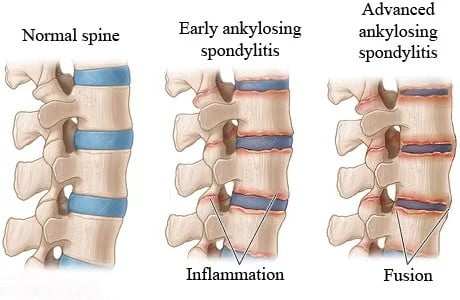
Overview | Ankylosing spondylitis (also known as axial spondyloarthritis) is an inflammatory disease that causes the fusion of vertebrae in the spine over time. This fusion reduces spinal flexibility and can lead to a hunched posture. If ribs are affected, breathing deeply becomes difficult. |
Types | – Ankylosing spondylitis: Visible on X-rays, characterized by vertebrae fusion. – Nonradiographic axial spondyloarthritis: Diagnosed based on symptoms, blood tests, and imaging. |
Symptoms | – Back pain and stiffness, especially in the morning or after inactivity. – Neck pain and fatigue. – Symptoms may worsen, improve, or occur irregularly. |
Commonly Affected Areas | – Joint between the base of the spine and the pelvis. – Vertebrae in the lower back. – Points where tendons and ligaments attach to bones (spine and back of the heel). – Cartilage between the breastbone and ribs. – Hip and shoulder joints. |
Diagnosis | – Physical exam assessing range of motion and pain. – X-rays (visible signs may not appear early). – MRI for nonradiographic cases. – No specific lab tests; HLA-B27 gene testing. |
Treatment | – Medications (NSAIDs, TNF blockers, IL-17 inhibitors, JAK inhibitors). – Physical therapy. – Surgery (if severe pain or hip joint damage). |
Self-Care | – Stay active. – Quit smoking. – Practice good posture. |
Coping and Support | – Understand condition variability. – Consider joining support groups. |
Preparing for Appointment | – Compile symptom details, personal information, and medication list. – Prepare questions for your doctor. |