Anal Fistula: An Overview
Anal fistula, medically known as fistula-in-ano, is a condition characterized by an abnormal tunnel connecting the internal anus to the skin surrounding the external anus. This condition typically arises following an infection in an anal gland, leading to an abscess that either drains spontaneously or requires surgical intervention.
The Formation of Fistulas
The persistence of the drainage channel post-abscess treatment results in the creation of a fistula, maintaining a connection between the previously infected gland or the anal canal and the skin’s surface.
Treatment Necessities
While surgical procedures are the standard treatment for anal fistulas, there are instances where non-surgical methods may be applicable.
Symptoms of Anal Fistulas
Individuals with an anal fistula may experience:
- An external opening near the anus
- Redness and inflammation around the fistula’s exterior
- Discharge of pus, blood, or fecal matter from the fistula
- Discomfort or pain in the anal region, exacerbated by sitting or defecation
- Fever as a sign of ongoing infection
Causes and Development
Anal fistulas typically originate from an anal gland infection, which leads to an abscess and subsequent drainage. The residual tunnel, or fistula, forms beneath the skin along the path of the drained abscess, linking the anal gland or canal to the skin.
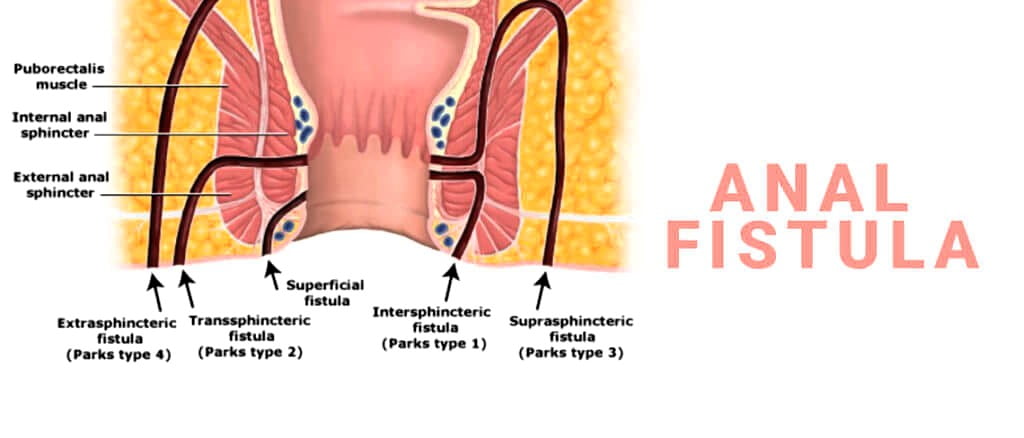
Sphincter Muscle Involvement
The anal sphincter muscles, responsible for stool regulation, are often implicated in fistula formation. The extent of their involvement is crucial for surgeons to determine the appropriate treatment strategy.
Risk Factors
Certain conditions increase the likelihood of developing an anal fistula, including:
- History of anal abscesses
- Inflammatory bowel diseases like Crohn’s disease
- Trauma or injury to the anal region
- Localized infections
- Anal cancer treatments, such as surgery or radiation
Anal fistulas are more prevalent in adults around 40 years of age but can also affect younger individuals, particularly those with Crohn’s disease. The condition is more common in males than females.
Potential Complications
Despite successful treatment, the recurrence of anal fistulas and abscesses is a possibility. One of the significant risks associated with surgical intervention is the potential for fecal incontinence, where control over bowel movements is compromised.
| Section | Subsection | Details |
|---|---|---|
| Anal Fistula Overview | Formation | Abnormal tunnel from an infected anal gland to the skin. |
| Treatment Necessity | Surgical intervention is standard; nonsurgical options may apply. | |
| Symptoms | Common Indicators | Discharge, pain, fever, and inflammation around the anus. |
| Causes | Origin | Infection in an anal gland leading to an abscess and fistula formation. |
| Sphincter Muscle Involvement | Classification based on sphincter muscle involvement aids treatment planning. | |
| Risk Factors | Common Risks | History of abscesses, inflammatory bowel diseases, trauma, infections, and anal cancer treatments. |
| Demographics | More common in adults around 40, especially males and those with Crohn’s disease. | |
| Complications | Recurrence and Incontinence | Possibility of recurrence and fecal incontinence post-treatment. |
| Diagnosis | Physical Exam | Inspection of the external and internal anal area. |
| Imaging Tests | MRI, endoscopic ultrasound, fistulography, and examination under anesthesia. | |
| Additional Tools | Fistula probe, anoscope, sigmoidoscopy/colonoscopy, and injected dye solution. | |
| Treatment | Surgical Options | Fistulotomy, endorectal advancement flap, LIFT, ostomy and stoma, muscle flap. |
| Nonsurgical Options | Seton placement, fibrin glue and collagen plug, medication for Crohn’s disease. | |
| Lifestyle and Home Remedies | Comfort Measures | Pain medication, warm sitz baths, dietary fiber, and avoiding straining. |
| Preparing for Appointment | Specialist Referral | Gastroenterologist or colon and rectal surgeon. |
| Pre-Appointment | Fasting instructions, symptom record, personal information, medication inventory. | |
| Questions for Provider | Causes, tests, condition duration, dietary suggestions, treatment recommendations. | |
| Doctor’s Questions | Symptom onset, severity, location, improvement/worsening factors, other medical conditions. |