Diagnosing Thalassemia
Early Signs and Confirmatory Tests
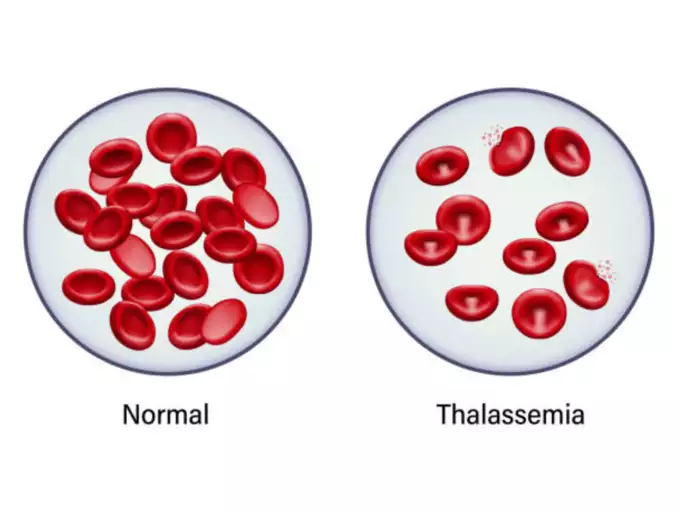
Children who may have moderate to severe thalassemia often exhibit symptoms within the first two years of life. If thalassemia is suspected, a doctor can use blood tests to confirm the diagnosis. These tests assess:
- The count and appearance of red blood cells.
- The size, shape, and color of these cells.
- DNA analysis to identify any genetic mutations responsible for thalassemia.
Prenatal Diagnosis
For early detection, prenatal testing can determine if an unborn child has thalassemia and the potential severity of the condition. The tests include:
Chorionic Villus Sampling (CVS)
Performed around the 11th week of pregnancy, CVS involves the collection of placental tissue to check for thalassemia.
Amniocentesis
Conducted around the 16th week of pregnancy, this test analyzes the amniotic fluid surrounding the fetus for signs of the disorder.
Treatment Options for Thalassemia
Managing Mild Thalassemia
Mild thalassemia traits typically do not necessitate any form of treatment.
Interventions for Moderate to Severe Thalassemia
For those with more pronounced forms of thalassemia, treatment strategies may include:
Regular Blood Transfusions
Severe thalassemia cases often require frequent blood transfusions, sometimes every few weeks. However, this can lead to an accumulation of iron in the bloodstream, which poses risks to the heart, liver, and other organs.
Chelation Therapy
Chelation therapy is essential for removing excess iron from the blood, which can accumulate from ongoing transfusions or naturally due to the condition itself. Maintaining iron levels is critical for health.
Oral medications like deferasirox (Exjade, Jadenu) or deferiprone (Ferriprox) are commonly prescribed. In some instances, deferoxamine (Desferal) is administered via injection.
Stem Cell Transplant
Also known as a bone marrow transplant, a stem cell transplant is a potential treatment for children with severe thalassemia. It aims to eliminate the need for continuous blood transfusions and medication to manage iron overload.
This procedure entails receiving stem cell infusions from a genetically compatible donor, often a sibling.
Self-Care and Support for Thalassemia
Self-Care Strategies
Proper self-care is crucial in managing thalassemia effectively:
- Avoid Iron Overload: Do not consume iron supplements unless prescribed.
- Nutrition and Supplements: Embrace a balanced diet rich in nutrients. Consult your doctor about taking folic acid and whether you need additional calcium and vitamin D.
- Infection Prevention: Maintain hygiene, avoid exposure to infections, and stay up-to-date with vaccinations like the annual flu shot, and vaccines for meningitis, pneumonia, and hepatitis B.
Coping Mechanisms and Support
Living with thalassemia can be demanding:
- Seek Professional Advice: Always reach out to your healthcare provider for any concerns or guidance.
- Join Support Groups: Connect with support groups for emotional support and valuable insights into managing thalassemia
Preparing for a Thalassemia Appointment
Essential Pre-Appointment Preparations
To ensure a productive consultation, consider the following steps:
Documenting Your Child’s Health
- Symptom Chronology: Note all symptoms observed, their onset, and any patterns.
- Family Medical History: Record any family incidence of thalassemia.
- Medication and Supplement Inventory: List all substances your child is taking, including dosages.
Questions for Your Doctor
Prepare a list of questions to gain clarity on your child’s condition, such as:
- Primary Concerns: What could be causing my child’s symptoms?
- Alternative Diagnoses: Are there other conditions that could be presenting similar symptoms?
- Diagnostic Tests: What type of testing is required?
- Treatment Options: What are the available treatments and your recommendations?
- Side Effects: What are common side effects of the suggested treatments?
- Comprehensive Care: How can thalassemia be managed alongside other health conditions?
- Dietary Guidance: Should we follow any specific dietary restrictions or supplement regimens?
- Educational Resources: Can you provide any literature or recommend informative websites?
Feel free to ask any additional questions that come to mind.
Expectations During the Appointment
Your doctor may inquire about:
- Symptom Consistency: Do the symptoms persist consistently or fluctuate?
- Symptom Severity: How intense are the symptoms?
- Relief Factors: Is there anything that alleviates the symptoms?
- Aggravating Factors: Have you noticed anything that exacerbates the symptoms?
| Category | Subcategory | Details |
|---|---|---|
| Overview | Definition | A genetic blood disorder causing less hemoglobin and resulting in anemia. |
| Management | Mild cases may not need treatment; severe cases require transfusions and lifestyle adjustments. | |
| Symptoms | Variability | Depends on thalassemia type and severity; can include fatigue, bone deformities, and more. |
| Age of Onset | Some at birth, others within the first two years, or may be asymptomatic carriers. | |
| Causes | Genetic Mutations | DNA mutations in cells making hemoglobin; passed from parents to children. |
| Alpha and Beta Chains | Mutations affect the production of these chains, leading to alpha or beta thalassemia. | |
| Risk Factors | Family History | Inherited through mutated hemoglobin genes. |
| Ancestry | More common in African Americans, Mediterranean, and Southeast Asian descent. | |
| Complications | Iron Overload | From the disease or frequent blood transfusions. |
| Infection | Increased risk, especially if the spleen is removed. | |
| Prevention | Genetic Counseling | Advised for those with thalassemia or carriers. |
| Reproductive Technology | Embryo screening combined with IVF for healthy babies. | |
| Diagnosis | Blood Tests | Reveal red blood cell count and abnormalities, DNA analysis for mutated genes. |
| Prenatal Testing | Chorionic villus sampling and amniocentesis to detect thalassemia in fetuses. | |
| Treatment | Blood Transfusions | For severe cases; can lead to iron buildup. |
| Chelation Therapy | To remove excess iron from the blood. | |
| Stem Cell Transplant | For severe cases, can eliminate the need for transfusions. | |
| Self-Care | Diet and Supplements | Avoid excess iron, ensure a healthy diet, and consider supplements like folic acid. |
| Infection Prevention | Good hygiene, vaccinations, and avoiding sick people. | |
| Support | Professional Advice | Reach out to healthcare providers for guidance. |
| Support Groups | For emotional support and information. | |
| Appointment Prep | Documentation | Record symptoms, family history, and medications. |
| Questions for Doctor | Inquire about causes, tests, treatments, dietary advice, etc. | |
| Doctor’s Questions | Be prepared to discuss symptom patterns and severity. |