Ampullary Cancer: An Overview
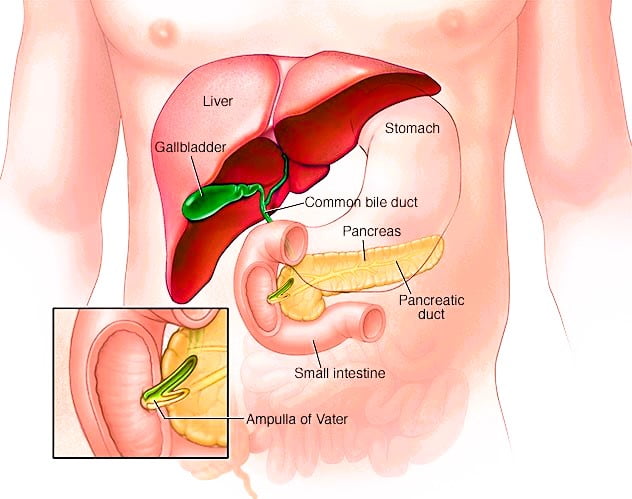
Ampullary cancer is a rare form of cancer originating from the cell growth in the ampulla of Vater, which is the junction where the bile and pancreatic ducts meet before emptying into the small intestine.
The Impact on the Digestive System
The cancer’s proximity to vital digestive organs like the liver, pancreas, and small intestine means that its growth can potentially affect these areas.
Treatment Modalities
The primary treatment for ampullary cancer typically involves surgical removal of the tumor. Additional therapies may include radiation and chemotherapy to target and destroy cancerous cells.
Recognizing the Symptoms
Ampullary cancer may present with symptoms such as:
- Jaundice (yellowing of the skin and eyes)
- Diarrhea
- Stools that are clay-colored
- Abdominal pain
- Fever
- Blood in the stool
- Nausea
- Vomiting
- Weight loss
When to Consult a Healthcare Professional
It’s advisable to seek medical attention if you experience any persistent symptoms that cause concern.
Understanding the Causes
The exact cause of ampullary cancer remains unknown. It occurs when cells in the ampulla of Vater undergo DNA mutations. These mutations disrupt the normal instructions for cell growth and death, leading to the rapid multiplication of cancer cells and the formation of a tumor. This tumor can invade and destroy healthy tissue and may eventually metastasize.
Risk Factors
Certain factors may elevate the risk of developing ampullary cancer, including:
- Age: It’s more prevalent in individuals over the age of 70.
- Genetic predispositions: Inherited DNA mutations associated with conditions like Lynch syndrome, familial adenomatous polyposis (FAP), and Peutz-Jeghers syndrome can increase the risk.
Prevention
Currently, there are no known preventive measures for ampullary cancer.
| Section | Key Points |
|---|---|
| Overview | – Rare condition with indeterminate external genitals<br>- Not a disease, but a disorder of sex development<br>- Usually identified at or shortly after birth |
| Symptoms | – Characteristics vary based on genetic sex (XX or XY)<br>- May include enlarged clitoris, closed labia, or undescended testicles |
| Causes | – Hormonal abnormalities during pregnancy<br>- Chromosomal and genetic factors<br>- Environmental influences |
| Risk Factors | – Family history of genital abnormalities or related genetic disorders<br>- History of unexplained infant deaths or reproductive issues |
| Complications | – Potential infertility<br>- Increased risk of certain cancers |
| Diagnosis | – Typically diagnosed at birth<br>- Involves family and medical history, physical exam, and various tests |
| Treatment | – Goal is psychological and social well-being, sexual function, and fertility<br>- May involve a team of specialists, medications, and surgery |
| Coping and Support | – Mental health support for families<br>- Importance of professional counseling and support groups |
| Preparing for Appointment | – Gather family history<br>- Bring support person<br>- Prepare questions for the doctor |