Alzheimer’s Disease Diagnosis: A Detailed Guide
Diagnosing Alzheimer’s disease is a comprehensive process that involves personal symptom reporting, corroborative information from close acquaintances, and a series of tests to evaluate cognitive function and identify brain changes.
Clinical Assessments:
- Physical and Neurological Exams: Healthcare professionals conduct physical exams and assess neurological health by testing reflexes, muscle strength, sensory perception, coordination, and balance.
Laboratory Tests:
- Blood Tests: These can exclude other causes of memory impairment, such as thyroid disorders or vitamin deficiencies. Some blood tests may measure beta-amyloid and tau proteins, although availability and insurance coverage for these tests may be limited.
Cognitive and Neuropsychological Tests:
- Mental Status Testing: Brief tests assess memory and thinking skills, while more extensive testing can provide a detailed cognitive profile.
Brain Imaging:
- MRI: Magnetic resonance imaging provides detailed brain images and can show brain region shrinkage associated with Alzheimer’s, as well as rule out other conditions.
- CT Scan: Computerized tomography offers cross-sectional brain images, commonly used to eliminate the possibility of tumors, strokes, or head injuries.
- PET Scans: These scans use radioactive tracers to visualize brain activity and can identify areas with reduced metabolism, amyloid plaque burdens, and tau tangles, although they are primarily used in research settings.
Advanced Testing:
- In certain cases, additional tests may measure amyloid and tau in cerebrospinal fluid, especially if symptoms are rapidly worsening or occurring at a younger-than-typical age.
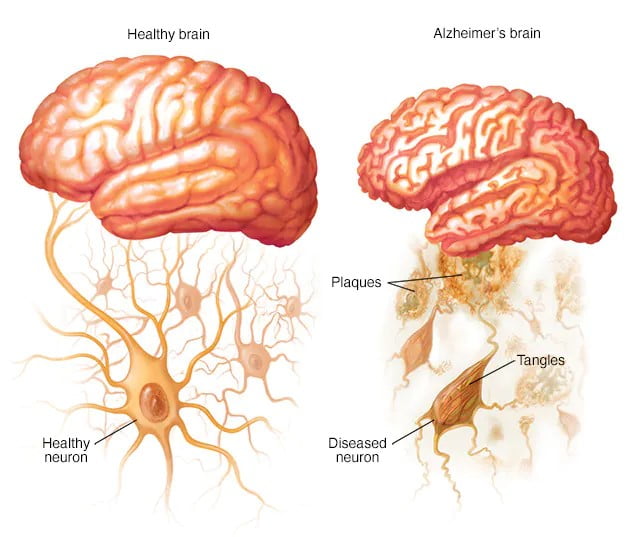
This diagnostic approach allows healthcare professionals to diagnose Alzheimer’s disease with increasing certainty during a patient’s lifetime, using biomarkers to detect the presence of plaques and tangles associated with the disease.
Future Diagnostic Approaches and Treatments for Alzheimer’s Disease
Diagnostic Innovations: Researchers are developing new tests to detect biological markers of Alzheimer’s disease in the brain. These advancements, including blood tests, aim to enhance diagnostic precision and potentially enable diagnosis before the onset of symptoms. A blood test for beta-amyloid levels is already in use.
Genetic Testing: While genetic testing is not routinely recommended for Alzheimer’s evaluation, it may be considered by individuals with a family history of early-onset Alzheimer’s. Consulting a genetic counselor is advised to weigh the pros and cons of genetic testing.
Treatment Options:
- Cholinesterase Inhibitors: These drugs boost intercellular communication by preserving a neurotransmitter that Alzheimer’s depletes. They often provide modest symptom improvement and are typically the first line of treatment. Common options include donepezil, galantamine, and rivastigmine, with side effects like gastrointestinal issues and sleep disturbances.
- Memantine: This medication slows symptom progression in moderate to severe Alzheimer’s and may be combined with cholinesterase inhibitors. Side effects are relatively rare but can include dizziness and confusion.
FDA-Approved Medications:
- Lecanemab (Leqembi): Approved in 2023 for mild Alzheimer’s and cognitive impairment, lecanemab slows cognitive decline by preventing amyloid plaque aggregation. Administered biweekly via IV, it can cause side effects ranging from infusion reactions to brain swelling and bleeding. The FDA advises MRI monitoring and genetic testing for the APOE e4 gene before and during treatment.
Ongoing Research:
- Lecanemab: Current studies are assessing its risks and effectiveness, particularly for individuals with a familial risk of Alzheimer’s.
- Donanemab: This investigational drug targets amyloid plaques and tau proteins and has shown promise in slowing cognitive and functional decline in early Alzheimer’s patients.
These developments represent a significant stride in the fight against Alzheimer’s, offering hope for earlier detection and more effective management of the disease.
Creating a nurturing and secure environment is essential for individuals with Alzheimer’s disease. Here are some strategies to support their well-being and maintain their functionality:
- Organize and Simplify: Keep everyday items like keys, wallets, and phones in a designated spot to prevent misplacement.
- Medication Management: Secure medications and use a checklist to monitor dosages.
- Financial Automation: Set up automatic payments and deposits for financial ease.
- Safety Measures: Equip the individual with a location-tracking mobile phone and program essential contacts.
- Home Security: Install sensors on doors and windows for added safety.
- Consistent Scheduling: Try to keep appointments consistent in timing and frequency.
- Visual Aids: Use calendars or whiteboards to help track daily activities and reinforce the habit of marking completed tasks.
- Home Safety: Remove unnecessary furniture and clutter to prevent falls and install handrails where needed.
- Appropriate Footwear: Ensure footwear provides adequate support and traction.
- Mirror Adjustment: Limit the number of mirrors to avoid confusion.
- Identification: Ensure the person always carries identification or wears a medical alert bracelet.
- Personalization: Surround them with meaningful photos and objects.
Regarding alternative medicine, while some supplements like Vitamin E, Omega-3 fatty acids, Curcumin, Ginkgo, and Melatonin are marketed for cognitive health, their effectiveness for Alzheimer’s treatment is not well-supported by research. It’s important to consult healthcare professionals before starting any new supplements, as they can interact with prescribed medications. Ongoing research continues to explore these and other potential treatments for Alzheimer’s disease. Always prioritize safety and work with healthcare providers to tailor a treatment plan that considers all medications and supplements being taken.
Lifestyle and Home Remedies for Alzheimer’s Disease
Maintaining a healthy lifestyle is beneficial not only for overall health but also for supporting brain health in individuals with Alzheimer’s disease.
Exercise: Regular physical activity is a key component of Alzheimer’s care. Simple exercises like walking can enhance mood, joint health, muscle strength, and heart health. Exercise also aids in sleep quality and digestive regularity. For those with mobility issues, stationary biking, resistance band exercises, or seated workouts can be good alternatives. Exercise resources are available on television, online platforms, or DVDs, especially those tailored for older adults.
Nutrition: Nutritional care is crucial as individuals with Alzheimer’s may neglect to eat or drink adequately, leading to dehydration and nutritional deficiencies. Ensuring access to healthy, easy-to-eat food options, encouraging regular fluid intake, and offering nutrient-dense shakes or smoothies can help maintain proper nutrition.
Social Engagement and Activities: Engaging in social and meaningful activities can support the retention of skills and contribute to overall well-being. Activities may include listening to music, dancing, reading, gardening, crafting, attending social events, or interacting with children.
Coping and Support: Alzheimer’s disease can evoke a range of emotions. Providing a supportive presence, reassurance, and respect for the individual’s dignity can aid in coping. A tranquil and consistent home environment helps minimize behavioral issues. Avoiding overstimulation and complex tasks can reduce anxiety and maintain clearer thinking.
Caregiver Support: Caregiving is demanding, and caregivers must also attend to their own well-being. This includes educating oneself about Alzheimer’s, seeking assistance from healthcare professionals, relying on friends and family for support, taking daily breaks, maintaining social connections, ensuring personal health, and joining support groups. Utilizing adult day centers and connecting with local Alzheimer’s support services can provide additional relief and resources.
These lifestyle and home remedies aim to create a supportive environment for those with Alzheimer’s and their caregivers, emphasizing the importance of self-care and community support.
Preparing for a medical appointment when experiencing memory loss or cognitive changes is crucial. Here’s a structured approach to ensure you cover all necessary details:
Before the Appointment:
Compile Medical Information:
- List all medical conditions, past and present.
- Gather information on family medical history, especially related to memory issues or dementia.
- Note down details of your medical team, including doctors and therapists.
- Prepare a list of all medications, including prescriptions, over-the-counter drugs, and supplements.
Document Symptoms:
- Record specific instances of memory lapses or changes in thinking skills.
- Note any daily activities that have become challenging.
During the Appointment:
- Expect Questions About:
- The nature and timeline of memory troubles.
- Any fluctuations in the severity of symptoms.
- Changes in daily activities, mood, and behavior.
- Medication usage and lifestyle habits like alcohol consumption.
- Physical symptoms such as tremors or mobility issues.
- Family history of memory problems or neurological conditions.
- Sleep patterns and any nocturnal activities.
Supporting Someone at Their Appointment:
- Be Ready to Share Observations:
- Offer insights into any behavioral changes you’ve noticed.
- Discuss any concerns about the person’s ability to manage tasks or safety while driving.
- Provide additional context to the symptoms they’ve described.
After the Appointment:
- Follow-Up:
- Ensure all prescriptions are understood and filled.
- Schedule any recommended tests or follow-up visits.
- Discuss the appointment with the person you’re supporting to ensure they understand the next steps.
Remember, being thorough and organized can help the healthcare professional make an accurate assessment and provide the best possible care plan.